
|
Otorhinolaryngology Otorhinolaryngology |
Sore throat
Differential diagnosis for a sore throat:
Tonsillitis
Peritonsillar abscess (Quinsy)
Supraglottitis / Epiglottitis
Deep neck space infections
-------
And the following that will be covered elsewhere in the curriculum:
Pharyngitis, common cold, foreign body, dental infections
.
Click on the golden tabs below to read about the topics...
Tonsillitis
Tonsillitis is inflammation of the pharyngeal tonsils. The inflammation usually extends to the lingual tonsils and adenoids therefore pharyngotonsillitis and adenotonsillitis are synonymous with tonsillitis

Aetiology
Most commonly viral - adenovirus, rhinovirus, RSV, EBV
15 - 30% are bacterial - mostly group A beta-hemolytic Streptococcus pyogenes (GABHS)
Epidemiology
- Tonsillitis most often occurs in children; however, the condition rarely occurs in children younger than 2 years
- Tonsillitis caused by Streptococcus species typically occurs in children aged 5-15 years
- Fever
- Sore throat
- Halitosis (foul breath)
- Dysphagia (difficulty swallowing)
- Odynophagia (painful swallowing)
- Mild airway obstruction e.g. mouth breathing
- Degree of respiratory distress
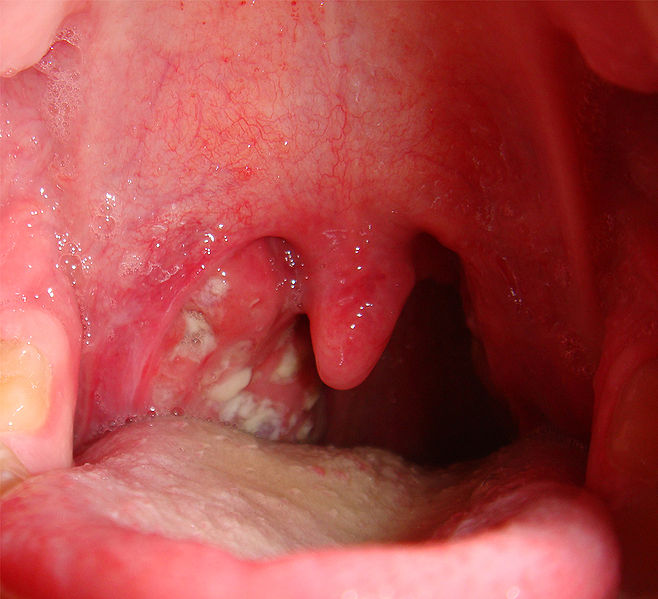
- Full examination of oral cavity including the oral mucosa, dentition, salivary ducts. In particular look for: tonsillar erythema, oedema +/- exudate (see pictures above)
- Tender cervical lymphadenopathy
- Flexible nasoendoscopy - especially if severe to assess for degree of airway obstruction
Possible complications of Streptococcal pharyngotonsillitis
Non-suppurative complications
Scarlet fever
Rheumatic fever
Post-streptococcal glomerulonephritis
Suppurative complications
Peritonsillar abscess (Quinsy)
Deep neck space infections
Cervical lymphadenitis
Management
1. ABC's
- Airway secured
- Fluid resuscitation
2. Antibiotics
- for acute inpatients - Penicillin IV 2MU Q6h
- for outpatients - Penicillin PO for 10 days
3. Steroids
Reserved for inpatients - usually Dexamethasone either 8mg stat or 8mg TDS for one day
4. Supportive therapy
- Anti-emetics
- Analgesia and antipyretics
EBV Tonsillitis
 Consider infectious mononucleosis particularly when tonsillitis is accompanied by:
Consider infectious mononucleosis particularly when tonsillitis is accompanied by:
- tender lymph nodes
- splenomegaly
- severe lethargy
- white/gray membrane may cover tonsils that are infected with EBV (see image)
However, EBV diagnosis can only be confirmed via blood tests. The importance of this is that EBV tonsillitis takes longer to resolve and patients should avoid contact sport
Peritonsillar Abscess (Quinsy)
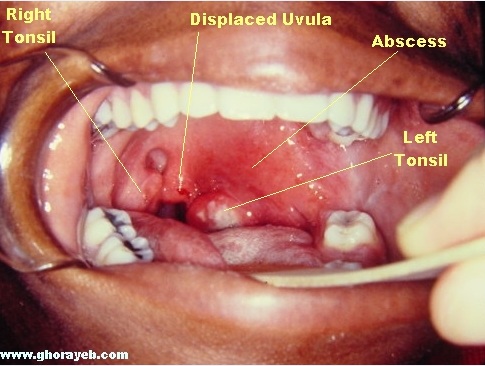
Each tonsil is surrounded by a capsule. It is in the potential space (peritonsillar space) between the tonsil and capsule that abscesses can form - a peritonsillar abscess, or in layman's terms, quinsy
IMPORTANT: the peritonsillar space is contiguous with several deeper spaces and infections can involve the parapharyngeal and retropharyngeal spaces (see deep neck space infections)
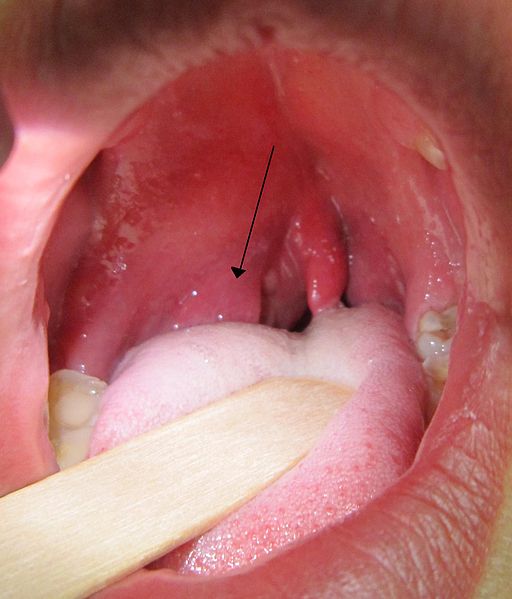
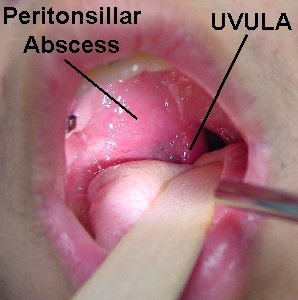
Compare these pictures above with the pictures shown in the tonsillitis section. What are the differences?
Note carefully the following:
- Uvula deviation to contralateral side
- Inferior and medial tonsil displacement
- Swelling of supratonsillar fold/soft palate rather than tonsil itself
______________________________________________________________________________
Aetiology
Tonsillitis can progress to cellulitis and then via tissue necrosis and pus formation to a peritonsillar abscess
or starts via an infection of minor salivary glands
Microbiology:
- A polymicrobial flora is isolated from peritonsillar abscesses
- Predominant organisms are anaerobes
- Aerobic organisms present are commonly Streptococci, S. aureus and H. influenzae
Epidemiology
Peritonsillar abscess (PTA) usually occurs in teens or young adults but may present earlier and occur in later adulthood
History
Symptoms are the same as for tonsillitis with a few other symptoms that are red flags for PTA and deep neck space infections:
- Neck pain
- Throat pain, more severe on the affected side +/- referred ear pain
- Trismus (lock-jaw) - due to inflammation of chewing muscles
- Voice change - in PTA pharyngeal oedema and trismus can cause a "hot-potato" voice - as if the patient is struggling with a mouthful of hot food
Remember: nasty dental infections can mimic PTA therefore examine the oral cavity carefully
Examination
As for tonsillitis
Apart from the visual findings as noted above:
- Drooling
- Trismus
- More severe dehydration
Some patients with quinsy require flexible nasoendoscopy to rule out epiglottitis
Investigations for tonsillitis and PTA
General:
1. FBC, U+E (especially if dehydrated)
2. Monospot test/heterophile antibody test - to rule out infectious mononucleosis
With PTA or if you suspect deep neck space infections:
1. Lateral neck X-ray
If clinically concerned or X-ray suggestive then proceed to CT scan
Management
Always think ABC's first: In severe circumstances endotracheal intubation or a surgical airway may be required
The cornerstone of PTA treatment is: incision and drainage
In addition the treatment regime includes the same medication and considerations as for tonsillitis
Patients with PTA tend to be more toxic - therefore require more IV fluid resuscitation (and greater care)
Trick question
What do you think this picture shows?
.
.
.
.
.
Answer: This is a patient who is day 3 post tonsillectomy. The white material you are seeing in the tonsillar fossae is healing mucosa - this will heal within weeks - it is NOT necessarily infected
Supraglottitis/Epiglottitis
Epiglottitis and supraglottitis are similar disease entities meaning:
inflammation of structures above the insertion of the glottis in the oropharynx including the epiglottis, vallecula, arytenoids and aryepiglottic folds (see picture below for nasoendoscopic view of the larynx)
The normal larynx:
.
1. Vocal cord
2. Vestibular ligament/fold
3. Epiglottis
4. Aryepiglottic fold
5. Corniculate cartilage
6. Piriform fossa
7. Lingual tonsil
Aetiology
Haemophilus influenzae type b (Hib) used to be responsible for >90% of epiglottitis cases
Due to vaccination the incidence has dropped markedly
Now other bacterial pathogens are responsible for the majority of cases including Streptococci, Staphylococcus and a number of gram negative bacilli
A Danish study demonstrated an incidence of paediatric epiglottitis of 4.9 cases per 100,000 per year in the decade before Hib vaccination.
With the introduction of widespread Hib vaccination - 1996 to 2005 - an incidence of only 0.02 cases per 100,000 per year was seen. (1)
History
- Sore throat
- Odynophagia/dysphagia
- Muffled voice - "Hot potato voice"
- Adults may have had a preceding upper respiratory tract infection (URTI)
Always ask about vaccination if you suspect supraglottitis
Examination
- "Toxic" appearance of patient
- Sitting or leaning forward. Extreme = "Tripod position" - Sitting up on hands, with the tongue out and the head forward
- Drooling/inability to handle secretions
- Irritability
- Stridor: A late finding indicating advanced airway obstruction
+ Muffled voice, cervical adenopathy, fever, respiratory distress, mild cough
Flexible nasendoscopy should be undertaken judiciously in children but may be required for diagnosis + assessment of airway (if the patient will tolerate it)
Remember: The progression of supraglottitis can be rapid (i.e. over hours!)
Investigation
Diagnosis is clinical but the following may be used as adjuncts
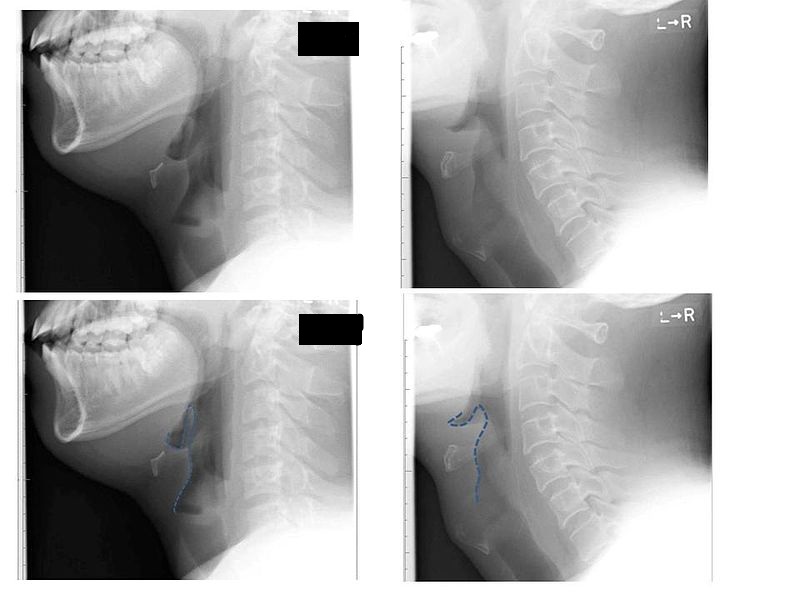
1. Lateral Neck XR - may be useful (see image below)
Most adults are stable and may safely undergo imaging
2. As mentioned above - judicious use of flexible nasoendoscopy
3. Blood cultures
Click for details |
This lateral neck X-ray demonstrates a classic radiographic finding in epiglottitis - the "thumb sign"
- This is due to swelling of the epiglottis
- The swelling of the epiglottis on the X-ray is shown by the blue dotted line - the left side is normal and the right has the abnormality
Management
1. Airway is the priority - ensure early ENT review. You should know where the surgical airway (cricothyrotomy) kit is
Unstable patients/severe respiratory distress may need immediate intubation or surgical airway management
If patient is stable they may still need monitoring in ICU
Minimise distress - particularly important in paediatric patients
2. Antibiotic - 1st choice is ceftriaxone (needs to be checked with local hospital policy)
3. Supportive therapy
Analgesia, anti-emetics, IV fluid



