Module 4: Cervical and breast screening
We are going to look at cervical and breast screening. The main focus will be on cervical screening as breast screening will be covered in more depth in your campus based learning block during the all day Interdisciplinary Women's Health seminar series.
You will also have already gained both practical experience of speculum examination and covered the importance of communication and interpersonal skills in your GTA (Gynaecology Teaching Associates) teaching. It is sometimes more difficult for males to obtain experience in intimate examinations of women and it is important that clinicians always have a chaperone present during these. As students you must always have a senior staff person present when doing intimate exams. When you do get the opportunity during this attachment to examine women make sure that you document what you have done in your log book in clinical examinations area.
You might also like to have a look again at your GTA booklet which is available on Canvas GTA Booklet.
What causes cervical and breast cancer? We don't really fully understand the answer to that question for breast cancer but we will be looking at some of the risk factors. However we now know that most cervical cancers are caused by oncogenic subtypes of Human Papilloma Virus (HPV). The subtypes mainly implicated are 16 and 18. We will be looking at some of the research around this during this week and talking about the HPV vaccine.
We are due to have a change regarding cervical screening in NZ- from 2020 NZ will change how it goes about cervical screening. It will now be 5 yearly instead of 3 yearly and will look for oncogenic HPV as the first screening tool. More information about this is available on the NSU website at HPV primary screening.
Screening programmes for both cervical and breast cancer are in place in New Zealand. We will also be looking at the National Screening Unit website to give us further information
If you would like to have a look at a brief review of the first 10 years of cervical screening then Cervical screening in New Zealand - a brief statistical review of the first decade gives a good overview.
The earliest cervical screening programme was started in Norway in 1959. Although cervical screening was being promoted in New Zealand in the 1950's the actual National Cervical Screening Programme (NCSP) wasn't launched until 1990. Since then there has been a 40% decrease in the incidence of cervical cancer.
Screening for breast cancer is carried out by BreastScreen Aotearoa and commenced in December 1998. In the first two years more than 58 per cent of eligible women have had mammograms through BreastScreen Aotearoa (BSA). During the same period 1184 cancers have been detected through the programme.
There are obviously some criteria that need to be met before implementing a screening programme for a disease. This table below gives you the WHO criteria.
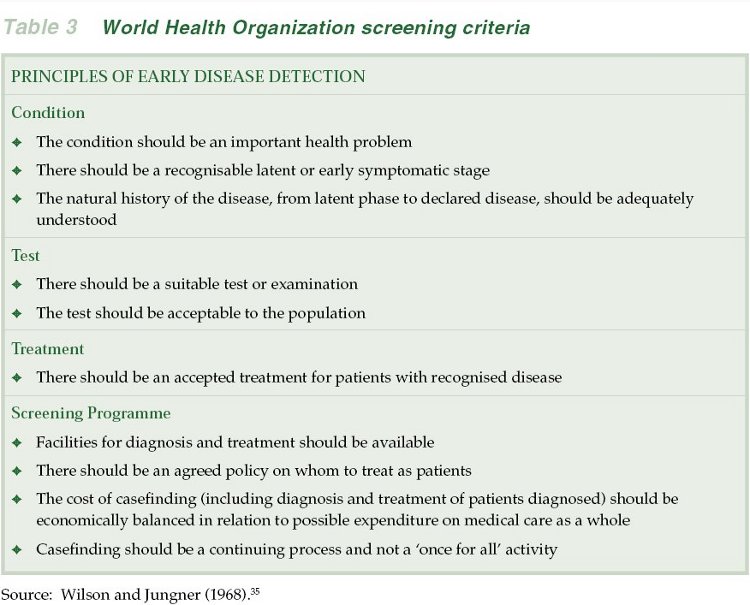
Cervical screening fits the WHO screening guidelines. Cervical cancer is preceded by cellular changes which can be detected by taking a sample from the cervix. Treating the abnormalities leads to the reduction in cervical cancer. With screening the chances of getting cervical cancer decreases to 1/570 women from 1/90 women without screening. Similarly with screening the chances of dying from cervical cancer decreases to 1/1280 women from 1/200 women without screening.
 Objectives
Objectives
On completion of this section you should be able to:
- Recognise the importance of areas such as gender issues, doctor-patient interaction, chaperone policies, socioeconomic and ethnic factors affecting women's health care
- Discuss the history of cervical screening in New Zealand
- Describe the contribution of Human Papilloma Virus (HPV) to the aetiology of cervical cancer
- Counsel women on the benefits and limitations of cervical and breast screening
- Counsel women on the HPV vaccine and the need for ongoing cervical screening
- Access MOH information for women on the various aspects of cervical and breast screening
- Describe what follow up is necessary if a smear result is abnormal
Cervical Screening Guidelines
The last objective is particularly relevant so one of the most important documents on the NSU website is the Cervical screening guidelines document . You may want to save your own personal copy for further reference as you will need to be able to tell women what to do if their smear report is abnormal.
 Readings
Readings
Roberts H. Gynaecology Teaching Associates (GTA). Information for medical students. Auckland: University of Auckland; 2017. GTA Booklet
National Screening Unit. Guidelines for cervical screening in New Zealand.
National Screening Unit. https://www.nsu.govt.nz
Look at
Lewis H. BPAC. Cervical smears- achieving equity. 2009. https://bpac.org.nz/BPJ/2009/September/docs/bpj23_csmears_pages46-55.pdf
Below are some readings that may of interest
New Zealand Cervical Cancer Audit. Cervical Cancer Audit report: Screening of women with cervical cancer, 2000-2002. Wellington: Ministry of Health; 2004.
Full text
Overcoming barriers to cervical screening in Pacific women. Best Practice J. 2010;32. Available from: http://www.bpac.org.nz/BPJ/2010/November/cervicalscreening.aspx
Full text
McFadden K, McConnell D, Salmond C, Crampton P, Fraser J. Socioeconomic deprivation and the incidence of cervical cancer in New Zealand: 1988-1998. N Z Med J. 2004;117(1206):U1172. Available from: http://www.nzma.org.nz/journal
Full text
McLeod M, Cormack D, Harris R, Robson B, Sykes P, Crengle S. Achieving equitable outcomes for Maori women with cervical cancer in New Zealand: health provider views. N Z Med J. 2011;124(1334):52-62. Available from: http://www.nzma.org.nz/journal
Full text
McLeod M, Harris R, Purdie G, Cormack D, Robson B, Sykes P, et al. Improving survival disparities in cervical cancer between Maori and non-Maori women in New Zealand: a national retrospective cohort study. Aust N Z J Public Health. 2010;34(2):193-9.
Full text
Kang YJ, Lewis H, Smith MA, Simonella L, Neal H, Bromhead C, et al. Pre-vaccination type-specific HPV prevalence in confirmed cervical high grade lesions in the Maori and non-Maori populations in New Zealand. BMC Infect Dis. 2015;15(1):365.
Full text
Kitchener HC. HPV primary cervical screening: time for a change. Cytopathology. 2015;26(1):4-6.
Full text
Images
Beischer NA, Mackay EV. Colour atlas of gynaecology [extracts]. Sydney: W.B. Saunders; 1981.
Lecturer's note: View images 40 (Nabothian cysts) & 303( Leukoplakia of cervix indicative of high grade CIN. Histology revealed carcinoma in situ).
Catalogue record for print book



