Cervical screening
 What do you need to discuss before doing a smear?
What do you need to discuss before doing a smear?
Before doing a smear check the relevant history eg menstrual history, pregnancy history,cervical smear history,any unusual discharge, using contraception. This is outlined in your GTA booklet. If this is the woman's first smear or she has not had one for many years you will need to explain 3 main areas:
What a smear test is looking for eg "A cervical smear test shows if there are abnormal changes in cells on the surface of the cervix"
Occasionally women are uncertain of the difference between having a smear test and having swabs taken to check for infection and the difference should be explained
Also women need to know that, like other screening tests, cervical screening is not 100% effective and that they need to seek advice if they have abnormal symptoms. This is outlined in the pamphlet for women - "cervical screening: what wāhine need to know" discussed on the next page
Exactly what you are going to do eg show woman the speculum and discuss insertion process. She needs to know that if at any stage she feels discomfort that she can ask you to stop the examination.
The cervical screening register: the woman needs to actively opt off by signing a form if she does not want her smear results to go to the register
 Where do you need to take the sample from?
Where do you need to take the sample from?
When you are taking a smear you need to know what a normal cervix looks like. Here are 2 pictures for you to look at. This first one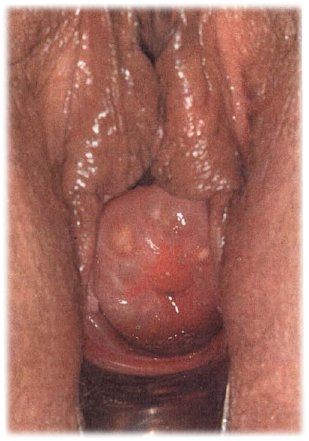 is actually a normal cervix and you can see a red area surrounding the extenal cervical os. The most peripheral extent of this red area is probably the squamo-columnar junction and therefore where you need to take your sample from. This is because cervical cancer can be squamous cell (80%) or adenocarcinoma (20%) so taking the sample from the junction means you will hopefully pick up any abnormal epithelial cells of either type. The squamous-columnar junction, SCJ is where the squamous cells on the peripheral ectocervix meet the columnar cells from the cervical canal. The white areas on this picture are Nabothian follicles-benign mucous retention cysts. You should now look again at the GTA booklet to remind you about sampling techniques and which samplers to use if the SCJ is not visible. Although we try to detect adenocarcinoma precancerous changes, cervical smears are better at detecting squamous change and screening has not effected such dramatic change on adenocarcinoma rates.
is actually a normal cervix and you can see a red area surrounding the extenal cervical os. The most peripheral extent of this red area is probably the squamo-columnar junction and therefore where you need to take your sample from. This is because cervical cancer can be squamous cell (80%) or adenocarcinoma (20%) so taking the sample from the junction means you will hopefully pick up any abnormal epithelial cells of either type. The squamous-columnar junction, SCJ is where the squamous cells on the peripheral ectocervix meet the columnar cells from the cervical canal. The white areas on this picture are Nabothian follicles-benign mucous retention cysts. You should now look again at the GTA booklet to remind you about sampling techniques and which samplers to use if the SCJ is not visible. Although we try to detect adenocarcinoma precancerous changes, cervical smears are better at detecting squamous change and screening has not effected such dramatic change on adenocarcinoma rates.
The second picture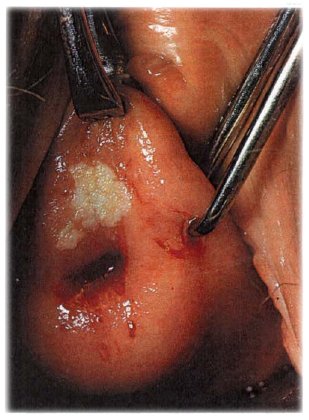 obviously looks abnormal and this in fact is a cervical cancer. Remember any cervix that looks abnormal should always be referred for colposcopy/second opinion even if the smear is normal.
obviously looks abnormal and this in fact is a cervical cancer. Remember any cervix that looks abnormal should always be referred for colposcopy/second opinion even if the smear is normal.
In New Zealand, smears are taken and processes using liquid based cytology, rather than the traditional "Pap" smear technique- this involved collecting the cells with a sampling device such as a spatula and smearing these cells onto a glass slide. Liquid based cystology reduces the risk of an unsatisfactory sample, requires a shorter time to interpret results, and enables a "co-test" for HPV on the same sample.
In Australia, this "Pap" test has been used up until December 2017, when Australia moved to HPV-based screening as a first-line test. If the test is HPV positive, liquid based cytology is then done on the sample.
If you are interested, this video outlines the changes that have happened in Australia's screening programme. New Zealand plans to change to a HPV based screening model by 2021.
 Who to screen, and how often
Who to screen, and how often
HPV is sexually transmitted and cervical screening is only necessary for women who are sexually active. In NZ cervical screening starts at age 20 even if the woman has been sexually active before this age. This is because HPV infections and any resulting dysplasia acquired since the onset of sexual activity will either have resolved by age 20 or will be picked up at the time of the first smear. Cervical cancer under the age of 20 is extremely rare.
If the first smear is normal, the 2nd one is done a year later to rule out the possibility of a false negative result. The rate of false negatives varies between 5-55% and they are due to errors in sampling, screening and interpretation. If results continue to be normal, screening is continued at 3 yearly intervals. If it has been more than 5 years since the previous smear the next one needs to be taken in 1 year before going back to 3 yearly smears. Screening continues until age 69, if a woman has a cervix. Women who have had a hysterectomy for benign reasons no longer require smears as long as their smears were normal in the 5 years preceding the hysterectomy. If the surgery was carried out because of cervical cancer or persistent dysplasia ongoing vault smears may be required.
The Cervical Screening Register
When you look at the Cervical Cancer Audit Report and this BPAC article you will see that that the screening history of the women in NZ who developed invasive cervical screening was not adequate - 80% had not had regular smears. At present in New Zealand women are invited to join NCSP and BSA when they are seen by their health practitioner. Women can also join BSA online in the National Screening Unit website. Health practitioners who provide cervical screening need to set up their own recall system for cervical smears as NCSP is only there as a back up to remind a woman who does not come for her smear within 3 months of the due date.
The Cervical screening register is an opt-off system. Practitioners need to ask women for permission to put their name on the register, as a result their smear results will be sent from the lab to the register automatically. If women do not wish this to happen they are required to sign an opt-off form. Once registered, the woman will get a letter to give her the result of her first smear, tell her when the next smear is due and to check her personal details are correct. Thereafter she will only be contacted by the register if her smear is abnormal or her smear is more than 3 months overdue. Once part of the register, a woman will have all her cytology, histology, colposcopy, and cervical treatments recorded and these will be accessible to practitioners registered with NCSP, such as susequent smear takers, colposcopists or cytologists.
The ‘register’ writes to the smear taker about 2 issues. Firstly, to provide feedback on the quality of smears that have been taken over a 6 or twelve month period eg number of inadequate samples. Secondly, they will contact the smear taker to request information on follow up eg for women who have not had a colposcopy after a smear result which would indicate colposcopy is necessary.
Smears are reported using the Bethesda reporting system.
Bethesda Reporting System
Smear results under this reporting system have 3 components
- adequacy of sample
- general categorisation and diagnosis
- recommendation on follow up
As a smear taker, it is important to think about how you will inform a woman about her smear results. Most smear takers usually only contact the woman if the results are abnormal. You need to think about good ways of explaining an abnormal result.
For example: "You have some changes in the cells on your cervix. Often these changes go away by themselves but in a small number of women, if the changes are left, they can become pre-cancerous. If we can remove the abnormal cells we can greatly reduce the chance of a cancer forming later"
Later on in this section we will be looking at how we follow up women with abnormal results.
Pamphlets for Women
If you are going to be involved with cervical and breast screening you need to know what resources there are for you to read and to give out. Both the cervical and breast screening areas of the National Screening Unit website have information about various aspects of screening. Women can be directed to these for information or they can be printed off from the screen. The "what wāhine need to know pamphlet" we have mentioned earlier is the NSU' and MOH's standard brochure to explain cervical screening.
How are smears and biopsies reported?
Cytological abnomalities are reported by grade:
- ASC-US: atypical squamous cells of undetermined significance
- LSIL: low grade squamous intraepithelial lesion / HPV
- ASC-H: Atypical squamous cells, high grade abnormality cannot be excluded
- HSIL: High grade squamous intraepithelial lesion - precancerous (the laboratory may suggest changes consistent with CIN2 or CIN3)
- Atypical Glandular cells (AGC), Adenocarcinoma in situ (AIS), or Adenocarcinoma
- Suspected invasion or SCC (squamous cell carcinoma)
Histological changes are reported as:
- HPV (high risk or low risk)
- CIN 1 Cervical Intraepithelial neoplasia grade 1
- CIN 2 Cervical Intraepithelial neoplasia grade 2
- CIN 3 Cervical Intraepithelial neoplasia grade 3
- Invasive squamous cell carcinoma
- Invasive adenocarcinoma
|
Click here to see a pictorial display of what these histological changes look like |
You can see as we move from low grade to high grade lesions the nucleus of the cell become larger and occupy most of the cell with fewer normal cells left above the basement membrane. Untreated approximately 30% of women with HSIL (CIN 2/3) would progress to invasive cervical cancer over 10 years. LSIL (CIN 1) carries only a small risk of malignant progression. It may progress to HSIL (CIN 2/3) but commonly resolves without treatment and you will see from the screening guidelines document that in young women LSIL is usually observed initially. The presence and persistence of LSIL into the thirties however suggests that the immune system has failed to clear the HPV and the follow up in this age group is different.
 Activity- What to do if the smear result is abnormal?
Activity- What to do if the smear result is abnormal?
The document that you will find useful is a concise table that Diagnostic MedLab have put together showing the use of HPV testing in 3 clinical situations.
Result | Advice |
1.Smear shows LSIL -age 25-No previous abnormal | Repeat smear in................. |
2. Smear shows LSIL-age 35-No previous abnormal | The lab will automatically organise a ......test. If this test is negative, repeat smear in ...... If this test is positive refer for ......... |
3. Histologically confirmed LSIL at colposcopy | Treatment is not recommended. Repeat smear in ..................Woman can return to routine 3 yearly screening if............................................................. |
4.Smear shows HSIL but normal colposcopy and histology (pg 49 )-no previous abnormal | How is HPV testing helpful here? |
5. Smear shows HSIL and histology confirms this.(pg 51)-no previous abnormal | Is the advice the same here as for Q4? |
6.Smear report shows atypical glandular cells -no previous abnormal | What should you do now? |
1. Repeat smear in 12 months
2. Offer a HPV test. If this test is negative, repeat smear in 12 months. If this test is positive refer for colposcopy
3. Treatment is not recommended. Repeat smear in 12 months and then at 24 months. Woman can return to routine 3 yearly screening if both of these smears are normal.
4. Do yearly hpv testing and smear and if negative for 2 consecutive years return to 3 yearly screening
5. After treatment of the high grade lesion the follow up answer is the same as 4
6. Refer for colposcopy
Colposcopy
 As you have seen in the activity table above some women may require referral for colposcopy and you will need to be able to explain the process to them. At colposcopy the cervix is examined under magnification and acetic acid and/or iodine stain is applied with biopsy of abnormal looking areas. These may need excision by LLETZ (large loop excision of the transformation zone ) laser cone or cold knife cone or ablation by laser.
As you have seen in the activity table above some women may require referral for colposcopy and you will need to be able to explain the process to them. At colposcopy the cervix is examined under magnification and acetic acid and/or iodine stain is applied with biopsy of abnormal looking areas. These may need excision by LLETZ (large loop excision of the transformation zone ) laser cone or cold knife cone or ablation by laser. 
This brochure explains to women what will happen at colposcopy- read it now.