Case preparation
Intermenstrual and postcoital bleeding

Intermenstrual bleeding is bleeding between periods. Postcoital bleeding occurs after intercourse. Both of these may be caused by cervical conditions such as cervical ectropion, cervical polyps, cervicitis or cervical cancer.
Cervical ectropion (pictured above) is more common in situations of increased estrogen such as pregnancy and in women on combined oral contraceptives. Cervical ectropion (or eversion as it may be called) is a normal occurrence with the transformation zone being visualised on the surface of the cervix and this may sometimes cause bleeding after sex. Cervicitis is inflammation of the cervix, often by infection. Chlamydia infection is a common cause of cervicitis and intermenstrual bleeding or spotting. Intermenstrual bleeding may also be secondary to hormonal contraception or be pregnancy related.
If you would like to have a concise overview of intermenstrual bleeding have a look at this website
https://patient.info/doctor/intermenstrual-and-postcoital-bleeding
Postmenopausal bleeding
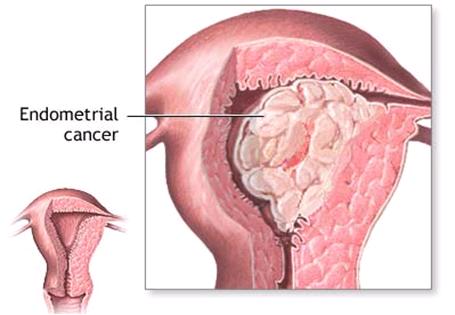 Periods stop at menopause. This may happen suddenly or over time with the periods becoming less frequent and eventually stopping. Accompanying symptoms of declining estrogen, such as hot flushes, are common. Any bleeding after 1 year with no periods is called postmenopausal bleeding. Although postmenopausal bleeding may be due to atrophic vaginitis (thinning of the vaginal mucosa due to estrogen withdrawal), endometrial or cervical polyps or due to hormone replacement therapy, it is always important to rule out carcinoma. Endometrial cancer is more common in older women. The first investigation here will be to do a vaginal ultrasound to check the endometrial thickness. The normal for a postmenopausal women is 5mm or less. If the USS shows a thickened endometrium then a pipelle biopsy will be the next investigation.
Periods stop at menopause. This may happen suddenly or over time with the periods becoming less frequent and eventually stopping. Accompanying symptoms of declining estrogen, such as hot flushes, are common. Any bleeding after 1 year with no periods is called postmenopausal bleeding. Although postmenopausal bleeding may be due to atrophic vaginitis (thinning of the vaginal mucosa due to estrogen withdrawal), endometrial or cervical polyps or due to hormone replacement therapy, it is always important to rule out carcinoma. Endometrial cancer is more common in older women. The first investigation here will be to do a vaginal ultrasound to check the endometrial thickness. The normal for a postmenopausal women is 5mm or less. If the USS shows a thickened endometrium then a pipelle biopsy will be the next investigation.
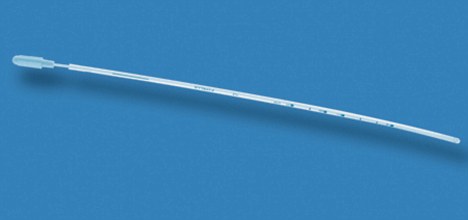
A pipelle (pictured) is a thin flexible tube that is passed through the cervix to take a small sample of the endometrium, via vacuum aspiration. It can produce a slightly crampy sensation as it is passed through the cervix but is generally well tolerated by patients and easy to perform in the clinic setting.
Menstrual disorders: Painful periods
This is one of other problems that may be associated with the menstrual cycle. Pain with periods may begin soon after menarche and is due to excess prostaglandins stimulating uterine contractions. This is called primary dysmenorrhoea and occurs in the absence of underlying organic pathology. This usually improves with age but NSAIDs are helpful, as is using the combined oral contraceptive pill. Painful periods that start later in life, often in the 3rd and 4th decade, is secondary dysmenorrhoea and is commonly associated with an underlying causative condition. To improve this the underlying cause needs to be treated. Have a think about what conditions may cause pain with periods later in life and then check with our list.
You may also like to look at the BMJ Best Practice reading for more information - Assessment of dysmenorrhea
![]() Click here to see possible causes
Click here to see possible causes
Secondary dysmenorrhoea can be caused by:
- Endometriosis
- Ovarian cysts
- Pelvic inflammatory disease (infection of the female reproductive organs)
- Uterine fibroids (noncancerous growths in the uterus)
- Intrauterine contraceptive devices (IUDs) Note: This refers to non-hormonal IUCDs. The mirena IUS is a hormone-releasing IUCD and due to its secretion of progesterone, can be a helpful treatment for pelvic pain and dysmenorrhoea.
- Scars inside the abdomen from previous surgery (adhesions)
- Tumors
- Inflammatory bowel disease



