Breastfeeding and lactation
We now know that the incidence and outcomes of diseases such as obesity, hypertension and cardiovascular disorders are associated with birth weight, growth, and feeding patterns. Over the last few decades the benefits of breast feeding for both the baby and the mother have been increasingly well documented. This section is going to look at these issues in more detail and give some advice about supporting women with breast feeding. If you have not already watched Simon Rowley's Introduction to the Neonate video, you should watch it now as it gives information on newborn feeding and calorie requirements: click to play, right click to download
What are the physiological steps that you have learned in Year 3 that cause lactation to commence? If you aren't sure, now is a good time to review the mechanisms behind lactation.
Supporting women to breast feed in the early postnatal period is crucial to success. There are many factors which can influence decisions whether to breastfeed or not, including socio-economic, cultural as well as maternal and infant. But evidence suggests that most women, regardless of ethnicity, will try to breastfeed for at least the first few days after delivery. Some, very common maternal reasons for discontinuing breastfeeding include:
Painful nipples
Engorgement
Under supply
Lactation consultants, as well as the LMC and midwives are available within most urban maternity units and are specifically trained to help with these sorts of issues related to breast feeding, However, the review article by Hoddinott highlights that if all hospital staff are providing support and incentives to mothers to both initiate and continue breastfeeding, the long term success rate of breastfeeding increases. This review also details many other barriers to breastfeeding and reasons why mothers have the problems listed above. The article by Castro et al. identifies groups of women in New Zealand who are less likely to breastfeed than others and some reasons for this. What do you think are the other factors involved here?
Implementation of the Baby Friendly Hospital Initiative is one of the measures designed to help: ‘train all health care staff in skills necessary to implement this policy’. More specifically, the policy recommends that every health professional working with mothers and infants be trained in the following areas: advantages of breastfeeding and the risks of not breastfeeding, how to achieve correct positioning and latching technique, hand expressing, how to address common breastfeeding problems, active listening skills and different teaching strategies. Health professionals also should be trained in working with mothers from a range of cultures, given the critical role culture plays in breastfeeding. This website is a good resource to review if you are interested in understanding more.
Providing in service training for all health professionals in breastfeeding and lactation management is now mandatory for all ‘Baby Friendly hospitals’. Given the influential role that health professionals have in supporting and promoting breastfeeding as a feeding choice to women, these in-service sessions are critical as there is strong evidence for the effectiveness of the positive impact that trained and skilled health professionals have on increasing initiation and duration.
The NZ Ministry of Health has two web sites devoted to breast feeding with information for Our work, for health practitioners and Your health: Breastfeding is perfect for you and your baby.
As you can see exclusive breast feeding is recommended until babies are around six months. This is in agreement with the WHO statement on breast feeding. Have a look at the review article by Hoddinott and the two Cochrane Reviews provided. You can see that exclusive breast feeding means breast milk only with no water, other fluids or solids and continues with the advice that supplemental breast feeding should continue for 2 years and beyond The NZ breast feeding website explains that exclusively breastfed infants can meet their fluid requirements with breastmilk and do not need water or any other drinks or food until around six months of age. After around six months of age, exclusive breastfeeding alone is not enough for baby to grow and develop - complementary foods (solids) should be introduced with breastfeeding continuing until at least one year or beyond."
 Activity
Activity
There are also benefits for mothers who breast feed one e.g. a reduction in premenopausal breast cancer. Have a look at the MOH website to see the other potential benefits for the mother. Table 2 in the Hoddinott review article also outlines some others. Have a think about what these may be. Mothers can look at the MOH web site list and view 7 benefits of breastfeed for their babies - how many can you think of?
Information on the website is:
- Breastmilk is easily digested and is free, always fresh and immediately available.
- A mother with a healthy diet provides breastmilk with a perfect blend of nutrients and protective antibodies (although it doesn't replace the need for immunisations).
- Breastfeeding helps baby grow and develop physically and emotionally
- Breastfeeding and breastmilk helps protect a baby from chest infections, meningitis, ear infections and urine infections.
- Breastfeeding decreases the risk of Sudden Unexpected Death in Infancy (SUDI).
- Breastfeeding and breastmilk may protect a baby from chronic tummy problems and some childhood cancers - there is also evidence of a reduced risk of allergies, eczema and asthma.
- Breastfeeding helps reduce the risk of obesity and may help reduce the risk of diabetes in baby's later life.
 The research behind these benefits
The research behind these benefits
If you would like to look at these benefits from a more medical viewpoint Table 1 in the Hoddinott review gives a good summary with details of the studies that the information has come from and the study quality. Have a look at this and find the quality of study and/or potential confounders for the following health benefits
- Acute otitis media
- Lower respiratory tract disease
- Obesity
- Diabetes
- Childhood leukaemias
- Sudden infant death syndrome
As you can see the research behind many of these benefits is of moderate or good quality.
 Can we prevent 1.3 million childhood deaths per year?
Can we prevent 1.3 million childhood deaths per year?
For developing countries breastfeeding is even more important as it can help reduce life threatening infections. Developing countries often have:
- Low immunisation rates
- Contaminated drinking water
- Reduced immunity because of malnutrition
The Hoddinott review estimates that exclusive breast feeding for 6 months and partial breast feeding extended to 1 year could prevent the deaths of 1.3 million children annually under the age of 5.
Lowbirthweight infants (<2500g) also benefit from reduced mortality and morbidity and breast feeding has a beneficial effect on neurodevelopment and growth.
Breastfeeding rates
The Hoddinott review points out that breast feeding rates have been low in UK and the US. How does NZ compare with these countries from your readings? One of the concerns is that there is a big decline in breast feeding in the first few days after birth, even though many of these mothers say they would have liked to continue. These figures emphasise the real benefit and need of support from staff such as midwives and lactation consultants and from doctors. A Cochrane review of 34 trials has shown that this support can increase the duration of breast feeding.
Showing women how to position the baby on the breast and correct positioning can help prevent nipple pain, poor milk supply and weight loss. The MOH website says that it is normal in the first 7 to 10 days for the nipples to be tender whilst breastfeeding is established. The area in and around the nipple is full of nerve endings which stimulate the brain to ‘let-down' the milk. However they go on to say that sore nipples that continue into the breastfeed are NOT normal and the main reason for the pain in the early days is generally attributable to incorrect positioning and latching.
 Activity- Is breast milk different from formula?
Activity- Is breast milk different from formula?
Click here to view the answer to the question above
The answer here would have to be a definite YES. As the Hoddinott review points out formula milk is "just food" whereas breast milk contains:
- Antibodies, particularly in the early colostrum
- Enzymes
- Hormones
New research into the contents of breast milk is continuing.
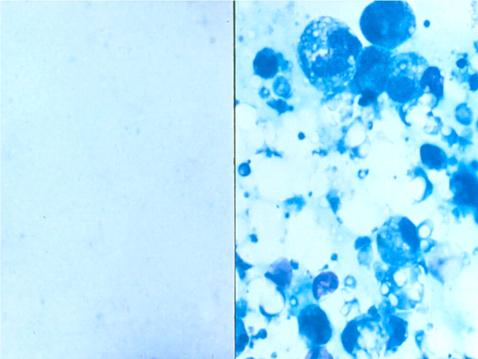
With breast milk being a complex living nutritional fluid it is obviously going to look different to formula milk. The picture below gives the appearance of both of these under the microscope. Which one do you think is breast milk?
Positioning and latching on
Positioning to get a successful latch is one of the most frequently asked questions for new mothers. Particularly, if there is engorgement, painful nipples or if the baby has jaundice. The MOH Our work: Breastfeeding website has connections to other useful websites eg La Leche League for videos on positioning and latching from birth. The MOH Your Health: Breastfeeding is perfect for you and your baby has videos and photos in sections How to breasttfeed and Problems with breastfeeding. This video is one of them, and there are others if you are interested.

Plunket also has helpful hints for new mothers with diagrams as well as video links.
 Drug safety in lactation
Drug safety in lactation
During your O&G attachment you may be asked about what medications are OK to use when a woman is breast feeding. Medicine use in lactation on the Medsafe website will be a useful resource for you in the future- it contains a good summary table of commonly used medications. Health Navigator also contains a good article for breastfeeding mothers on breastfeeding and medications. The NZ formulary has now included pregnancy categories for both pregnancy and lactation on its website- specific drugs can be checked here.
Have a look at these and then answer these questions:
Other common questions
The MOH website has a lot of helpful information in their section on Problems with breastfeeding for specific concerns that mothers may have. There are also links to the Youtube channel which contains all 7 chapters of the breastfeeding naturally video (you have seen the third chapter above).
Take some time now to review the information on:
- Painful nipples and engorgement
- Blocked milk ducts and mastitis
- Concerns about supply
There is also useful information on healthy eating and lifestyle. The Health Navigator page also gives some information on caffiene and alcohol intake recommendations in breastfeeding. Table 3 in the Hoddinott review also provides useful information on common problems in breastfeeding.
 Activity : Prevention and management of breast feeding problems
Activity : Prevention and management of breast feeding problems



