PALS Electrical therapy
- Defibrillators
- Manual external defibrillator
- Manual internal defibrillator
- Automated External Defibrillator
- Implantable cardioverter-defibrillator (ICD
- Electrodes
- Waveforms
- Trancutaneous pacing
- Transvenous / Implantable pacemakers
- Cardiversion
Defibrillators
Defibrillation is a common treatment for life-threatening cardiac arrhythmias, ventricular fibrillation and pulseless ventricular tachycardia. Defibrillation consists of delivering a therapeutic dose of electrical energy to the affected heart with a device called a defibrillator. This depolarizes a critical mass of the heart muscle, terminates the arrhythmia, and allows normal sinus rhythm to be reestablished by the body's natural pacemaker, in the sinoatrial node of the heart. Defibrillators can be external, transvenous, or implanted, depending on the type of device used or needed. Some external units, known as automated external defibrillators (AEDs), automate the diagnosis of treatable rhythms, meaning that lay responders or bystanders are able to use them successfully with little, or in some cases no training at all.
Study the diagram below for clarification:
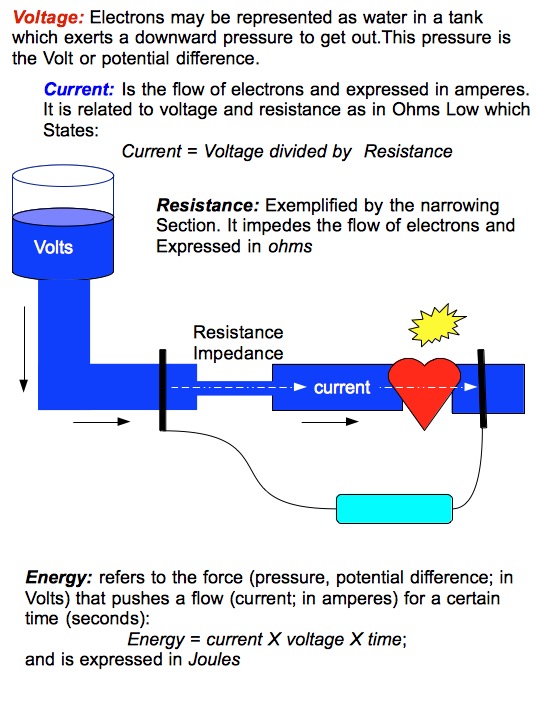
Physics
Energy: Energy in a defibrillator is expressed in joules. A joule is the unit of work associated with one amp of current passed through one ohm of resistance for one second.
When we express it in a formula, it is generally stated as follows:
Joules (Energy) = Voltage X Current X Time
Joules have become a surrogate for current in modern defibrillator language.
Current: Current is what actually defibrillates the heart. It is also expressed as Voltage/Impedance (resistance).
Impedance: Resistance to Flow; there is resistance in the electrical circuit itself as well as in the patient. The amount of impedance in a patient is difficult to determine as it relates to body mass, temperature, diaphoresis quality of the contact with paddles or pads. Impedance is expressed in ohms.
Manual external defibrillator
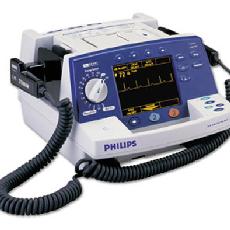
The units are used in conjunction with (or more often have inbuilt) electrocardiogram readers, which the healthcare provider uses to diagnose a cardiac condition (most often fibrillation or tachycardia although there are some other rhythms which can be treated by different shocks)
The healthcare provider will then decide what charge (in joules) to use, based on proven guidelines and experience, and will deliver the shock through paddles or pads on the patient's chest. As they require detailed medical knowledge, these units are generally only found in hospitals and on some ambulances. For instance, every NHS ambulance in the United Kingdom is equipped with a manual defibrillator for use by the attending paramedics and technicians. In the United States, many advanced EMTs and all paramedics are trained to recognize lethal arrhythmias and deliver appropriate electrical therapy with a manual defibrillator when appropriate.
|
Philips HeartStart XL Defibrillator |
Manual internal defibrillator

They are virtually identical to the external version, except that the charge is delivered through internal paddles in direct contact with the heart. These are almost exclusively found in operating theatres, where the chest is likely to be open, or can be opened quickly by a surgeon.
Please click the link to watch the video: https://www.youtube.com/watch?v=pB2z6yEpAqE
Automated External Defibrillator
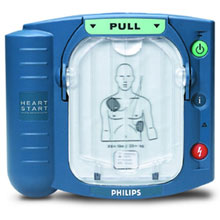
An automated external defibrillator or AED is a portable electronic device that automatically diagnoses the potentially life-threatening cardiac arrhythmias of ventricular fibrillation and ventricular tachycardia in a patient, and is able to treat them through defibrillation, the application of electrical therapy which stops the arrhythmia, allowing the heart to reestablish an effective rhythm.
These simple-to-use units are based on computer technology which is designed to analyze the heart rhythm itself, and then advise the user whether a shock is required. They are designed to be used by laypersons, who require little training to operate them correctly. They are usually limited in their interventions to delivering high joule shocks for VF (ventricular fibrillation) and VT (ventricular tachycardia) rhythms, making them generally of limited use to health professionals, who could diagnose and treat a wider range of problems with a manual or semi-automatic unit.
The automatic units also take time (generally 10–20 seconds) to diagnose the rhythm, where a professional could diagnose and treat the condition far more quickly with a manual unit. These time intervals for analysis, which require stopping chest compressions, have been shown in a number of studies to have a significant negative effect on shock success. This effect led to the recent change in the AHA defibrillation guideline (calling for two minutes of CPR after each shock without analyzing the cardiac rhythm) and some bodies recommend that AEDs should not be used when manual defibrillators and trained operators are available.
Automated external defibrillators are generally either held by trained personnel who will attend incidents, or are public access units which can be found in places including corporate and government offices, shopping centres, airports, restaurants, casinos, hotels, sports stadiums, schools and universities, community centres, fitness centres and health clubs.
|
AED |
Implantable cardioverter-defibrillator (ICD

Also known as automatic internal cardiac defibrillator (AICD). These devices are implants, similar to pacemakers (and many can also perform the pacemaking function). They constantly monitor the patient's heart rhythm, and automatically administer shocks for various life-threatening arrhythmias, according to the device's programming. Many modern devices can distinguish between ventricular fibrillation, ventricular tachycardia, and more benign arrhythmias like supraventricular tachycardia and atrial fibrillation. Some devices may attempt overdrive pacing prior to synchronised cardioversion. When the life-threatening arrhythmia is ventricular fibrillation, the device is programmed to proceed immediately to an unsynchronized shock.
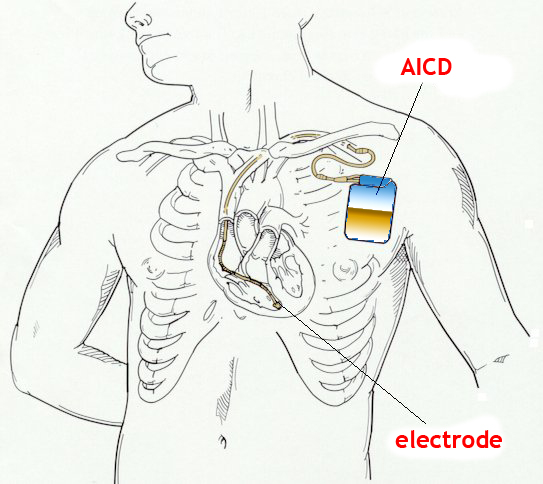
There are cases where the patient's ICD may fire constantly or inappropriately. This is considered a medical emergency, as it depletes the device's battery life, causes significant discomfort and anxiety to the patient, and in some cases may actually trigger life-threatening arrhythmias. Some emergency medical services personnel are now equipped with a ring magnet to place over the device, which effectively disables the shock function of the device while still allowing the pacemaker to function (if the device is so equipped). If the device is shocking frequently, but appropriately, EMS personnel may administer sedation.
Electrodes
Paddle electrodes

The most well-known type of electrode (widely depicted in films and television) is the traditional metal paddle with an insulated (usually plastic) handle. This type must be held in place on the patient's skin with approximately 25 lbs of force while the shock is delivered. while a shock or a series of shocks is delivered.
Paddles offer a few advantages over self-adhesive pads. Many hospitals in the United States continue the use of paddles, with disposable gel pads attached in most cases, due to the inherent speed with which these electrodes can be placed and used. This is critical during cardiac arrest, as each second of nonperfusion means tissue loss. Modern paddles allow for monitoring (electrocardiography), though in hospital situations, separate monitoring leads are often already in place.
Paddles are reusable, being cleaned after use and stored for the next patient. The gel is therefore not pre-applied and must be added before these paddles are used on the patient. Paddles are generally only found on the manual external units. Paddles require approximately 25 lbs of force to be applied while the shock is delivered.
Self-adhesive electrodes

Newer types of resuscitation electrodes are designed as an adhesive pad, which includes either solid or wet gel. These are peeled off their backing and applied to the patient's chest when deemed necessary, much the same as any other sticker. The electrodes are then connected to a defibrillator, much as the paddles would be. If defibrillation is required, the machine is charged, and the shock is delivered, without any need to apply any additional gel or to retrieve and place any paddles.
Most adhesive electrodes are designed to be used not only for defibrillation but also for transcutaneous pacing and synchronized electrical cardioversion. These adhesive pads are found on most automated and semi-automated units and are replacing paddles entirely in non-hospital settings. In the hospital, for cases where cardiac arrest is likely to occur (but has not yet), self-adhesive pads may be placed prophylactically.
Pads also offer an advantage to the untrained user, and to medics working in the sub-optimal conditions of the field. Pads do not require extra leads to be attached for monitoring, and they do not require any force to be applied as the shock is delivered. Thus, adhesive electrodes minimize the risk of the operator coming into physical (and thus electrical) contact with the patient as the shock is delivered by allowing the operator to be up to several feet away. (The risk of electrical shock to others remains unchanged, as does that of shock due to operator misuse.) Self-adhesive electrodes are single-use only. They may be used for multiple shocks in a single course of treatment, but are replaced if (or in case) the patient recovers then reenters cardiac arrest.
Placement
Resuscitation electrodes are placed according to one of two schemes. The anterior-posterior scheme (conf. image) is the preferred scheme for long-term electrode placement. One electrode is placed over the left precordium (the lower part of the chest, in front of the heart). The other electrode is placed on the back, behind the heart in the region between the scapula. This placement is preferred because it is best for non-invasive pacing.
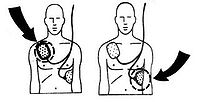
The anterior-apex scheme can be used when the anterior-posterior scheme is inconvenient or unnecessary. In this scheme, the anterior electrode is placed on the right, below the clavicle. The apex electrode is applied to the left side of the patient, just below and to the left of the pectoral muscle. This scheme works well for defibrillation and cardioversion, as well as for monitoring an ECG.
Waveforms
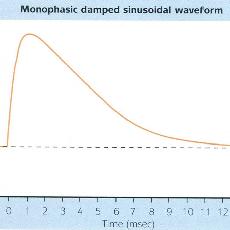
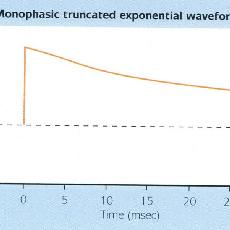
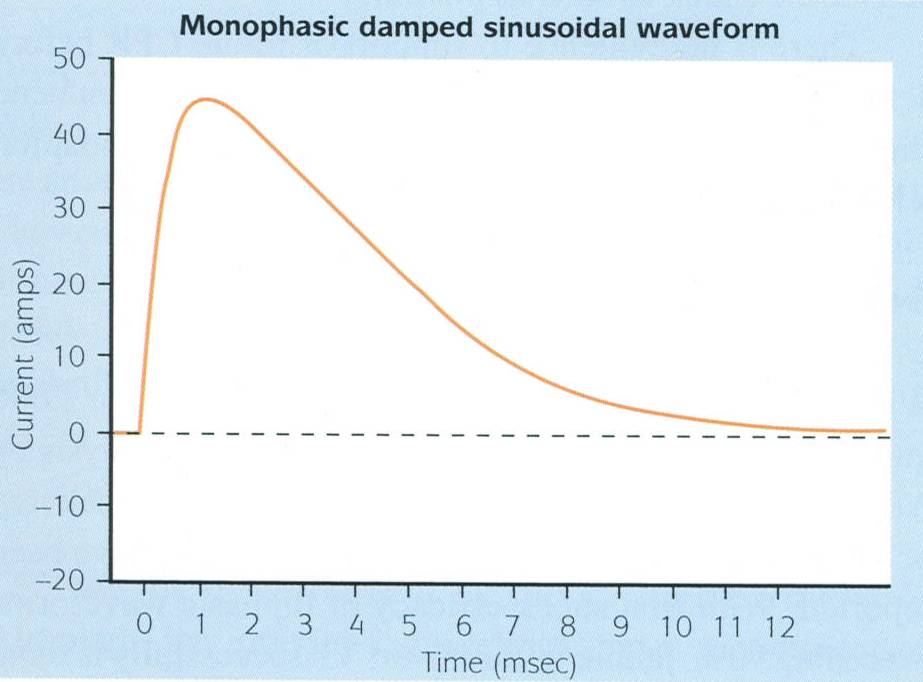
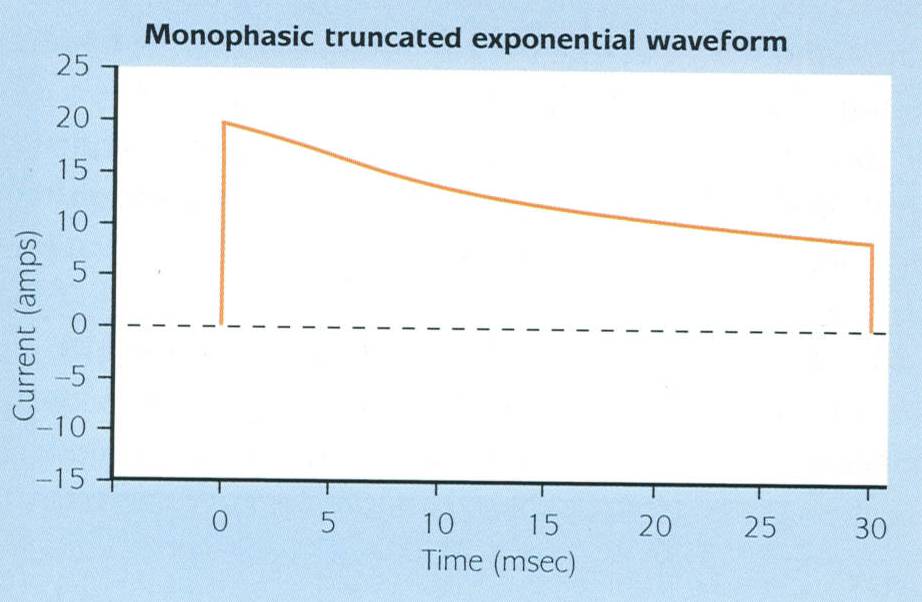
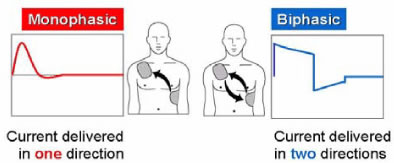
Monophasic Waveforms: A type of defibrillation waveform where a shock is delivered to the heart in one direction. It is shown graphically as current vs. time.
In this waveform, there is no ability to adjust for patient impedance, and it is generally recommended that all monophasic defibrillators deliver 360J of energy in adult patients to ensure maximum current is delivered in the face of an inability to detect patient impedance.
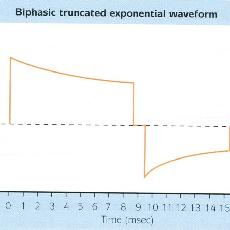
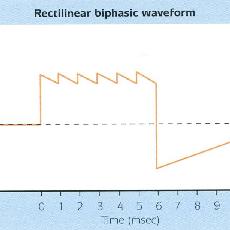
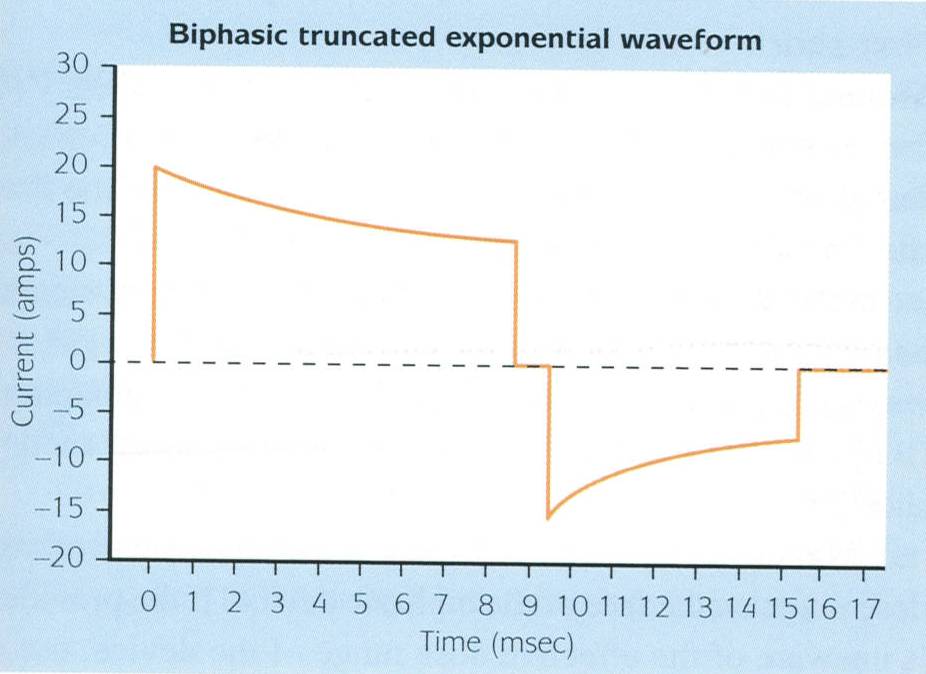
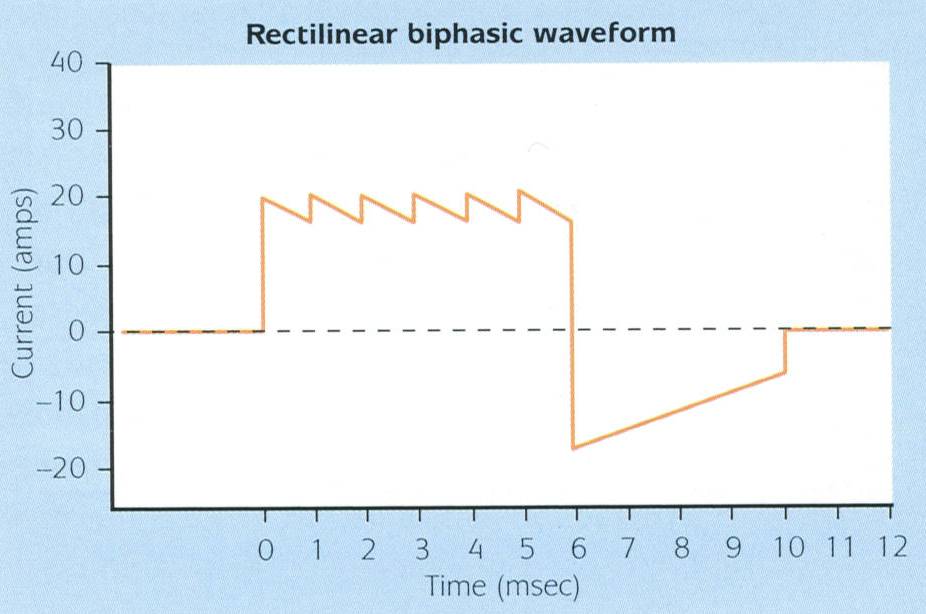
Biphasic Waveforms: A type of defibrillation waveform where a shock is delivered to the heart in two directions. Biphasic waveforms were initially developed for use in implantable defibrillators and have since become the standard in external defibrillators.
 Source: http://www.quickmedical.com/defibrillator/philips/biphasic_technology.html
Source: http://www.quickmedical.com/defibrillator/philips/biphasic_technology.html
While all biphasic waveforms have been shown to allow termination of VF at a lower current than monophasic defibrillators, there are two types of biphasic waveforms used in external defibrillators. These are shown below.
Please click on the images below to see a larger display.
|
Monophasic |
Monophasic |
Biphasic |
|
Biphasic |
Please Note:
It is really not appropriate to try to compare manufacturers’ biphasic waveforms as each is appropriate for the device in which it is found and none has been shown to be superior to others despite a number of clinical trials.
Trancutaneous pacing
Indications
Transcutaneous pacing (TCP) is indicated as a temporal measure for treatment of symptomatic bradycardias, including sinus bradycardias and atrioventricular (AV) nodal blocks.
Transcutaneous pacing is not beneficial in the treatment of asystole. You need a viable myocardium to pace.
Pad application
Pacemaker pads often applied "front/back" on a dry skin over the apex and just medial to the left scapula posteriorly. It may be necessary to shave excessive body hair to ensure good contact between the electrodes. Pads should not be applied to medication patches, ECG dots, and implantable devices.
Pacemaker setup
For most patients, the heart rate should be set to 70-80 bpm. The current should initially be set to zero milliamperes (mA). The pacemaker unit is then turned on, and the current is increased in 10-mA increments until capture is achieved.
Synchronous vs asynchronous modes
In the asynchronous or fixed-rate mode, the TCP delivers an electrical stimulus at preset intervals, independent of intrinsic cardiac activity. In theory, this could induce arrhythmias if stimulation occurs during the vulnerable period of the cardiac cycle (repolarization of the ventricle; R on T). Synchronous pacing is a demand mode in which the pacer fires only when no complex is sensed for a predetermined amount of time. Pacing generally should be started in the synchronous mode.
Minimizing discomfort
Pain from modern TCPs is related primarily to contraction of the pectoralis major skeletal muscle. Coughing and hiccups may occur secondary to stimulation of the diaphragm and thoracic muscles. This can be minimized by proper anterior pad placement, specifically, just medial to rather than directly over the left pectoral muscle, the other pad applied just medial to the left scapula posteriorly; and by using the minimum current necessary to ensure electrical capture.
As a general rule, pain is directly related to the amount of current delivered and inversely related to the skin surface area over which it is delivered. Thus, pain is minimized by using electrodes with large surface areas. Pain levels typically plateau once the electrode surface area exceeds 10 cm2. Most commercially available electrodes are 80-100 cm2.
Sedation with a short-acting agent, such as midazolam, an intravenous analgesia with an opiate, or both should be considered if the clinical situation permits their use.
Complications
Few complications are associated with the use of TCP. Skin burns have been reported with prolonged use.
Failure to capture
This is not the desired clinical outcome. Potential causes include:
- improper pad placement (directly over the sternum, scapula, or thoracic spine),
- poor skin contact (excessive hair, wet skin, or pad loosely applied),
- inadequate current output, and faulty or improperly set-up equipment.
- Anatomic barriers to current delivery may include fluid (pericardial effusion) or air (pneumothorax, chronic obstructive pulmonary disease [COPD]).
Hemodynamics in TCP
The atrial pacing threshold in humans is generally much higher than that for the ventricles; thus, current needed to stimulate all 4 chambers is not tolerated, even by patients who are sedated. This results in loss of the "atrial kick" and a reduction in cardiac output. Thus, external pacing may need higher pulse rate settings than expected in patients with symptomatic bradycardia to ensure that an adequate blood pressure is achieved.
CO (cardiac output) = HR (heart rate) X SV (stroke volume)
TCP Electrophysiology Explained
- Pulse duration
The modern TCPs use a long electrical pulse duration. Early TCPs used short (1-2 msec) impulses, more closely resembling the action potential duration of skeletal muscle rather than cardiac muscle (20-40 msec). This may preferentially stimulate skeletal muscle with resultant patient discomfort.
It has been found that increasing the duration from 1 msec to 4 msec caused a 3-fold reduction in threshold (the current required for stimulation). Increasing the pulse duration from 4 msec to 40 msec further halves the threshold, but longer durations produce no additional advantage. Current TCPs deliver between 20-40-msec pulses.
- Current
Using a longer pulse duration and larger electrodes permit patients to tolerate higher applied current. The average current necessary for external pacing ranges from about 50-100 milliamperes (mA).
One hundred mAs applied to an average chest with 50-ohm resistance for 20 msec delivers 0.1 Joules. This is well below the 1-2 Joules required to cause an uncomfortable tingling sensation in the skin. At these low levels of current delivery, it is the force of skeletal muscle contraction, not the electric current itself that determines the amount of discomfort.
http://emedicine.medscape.com/article/780639-overview#aw2aab6b5

|
Trans-cutaneous pacing
|
Transvenous / Implantable pacemakers
Types of Transvenous/Implantable pacemakers
• Unipolar pacemakers:
Permanent leads are either unipolar (where a single contact is made with the heart) or bipolar.
Unipolar systems (ventricular) are used in cases where atrioventricular (AV) conduction is likely to return.
When there are normal AV conduction and a sinoatrial (SA) disorder, then the pacing wire is situated in the right atrium.
• Dual-chamber pacemakers:
Have pacing electrodes in both the right atrium and the right ventricle.
They allow maintenance of the physiological relationship between atrial and ventricular contraction and also allow the paced heart to follow the increase in sinus rate that occurs during exercise.
• Dual-site atrial pacing:
Newer pacing systems have 2 atrial leads, one in the right atrial appendage and the other either in the coronary sinus or at the os of the coronary sinus.
The ventricular lead is in the right ventricle, either at the apex or at the outflow tract.
This system has been proposed as a promising treatment option for prevention of paroxysmal atrial fibrillation
• Biventricular pacemakers:
Pacemaker leads are placed in the right atrium, right ventricle and left ventricle.
Useful in the management of patients with heart failure who have evidence of abnormal intraventricular conduction (most often evident as left bundle branch block (LBBB) on ECG) which causes deranged ventricular contraction or dyssynchrony.
• Implantable cardioverter defibrillators (ICDs - combined with an internal defibrillator):
Designed to treat a cardiac tachyarrhythmia directly.
If a patient has a ventricular defibrillator and the device senses a ventricular rate that exceeds the programmed cut-off rate of the defibrillator, the device performs cardioversion/defibrillation.
Alternatively, the device, if so programmed, may attempt to pace rapidly for a number of pulses, usually around 10, to attempt pace-termination of a ventricular tachycardia.
Pacemaker codes
The North American Society of Pacing and Electrophysiology and the British Pacing and Electrophysiology Group have developed a code to describe various pacing modes. It usually consists of three letters, but some systems use four or five:
• Letter 1: chamber that is paced (A = atria, V = ventricles, D = dual-chamber).
• Letter 2: chamber that is sensed (A = atria, V = ventricles, D = dual-chamber, 0 = none).
• Letter 3: response to a sensed event (T = triggered, I = inhibited, D = dual - T and I, R = reverse).
• Letter 4: rate-responsive features; an activity sensor, e.g. an accelerometer in the pulse generator, in single or dual-chamber pacemakers detects bodily movement and increases the pacing rate according to a programmable algorithm (R = rate-responsive pacemaker).
• Letter 5: Anti-tachycardia facilities.
A pacemaker in VVI mode denotes that it paces and senses the ventricle and is inhibited by a sensed ventricular event. The DDD mode denotes that both chambers are capable of being sensed and paced.

|
Transvenous pacing
|
Cardiversion
Cardioversion is a medical procedure by which an abnormally fast heart rate (tachycardia) or cardiac arrhythmia is converted to a normal rhythm using electricity or drugs. Synchronized electrical cardioversion uses a therapeutic dose of direct electric current to the heart at a specific moment in the cardiac cycle.
The DC electrical discharge is synchronized with the R or S wave of the QRS complex. Synchronization in the early part of the QRS complex avoids energy delivery near the apex of the T wave which coincides with a vulnerable period for induction of ventricular fibrillation. (The peak of the T wave represents the terminal portion of the refractory state when adjacent heart fibres are in differing states of repolarization).
Transient delivery of electrical current causes a momentary depolarization of most cardiac cells allowing the sinus node to resume normal pacemaker activity. In the presence of reentrant-induced arrhythmias, such as paroxysmal supraventricular tachycardia (PSVT) and ventricular tachycardia (VT), electrical cardioversion interrupts the re-entrant circuits and restores a sinus rhythm.
Electrical cardioversion is much less effective in treating arrhythmia caused by increased automaticity (eg, digitalis-induced tachycardia, catecholamine-induced arrhythmia) since the mechanism of the arrhythmia remains after the arrhythmia is terminated and therefore is likely to recur.
Indications for electrical cardioversion:
Based on advanced cardiovascular life support guidelines, any patient with narrow or wide QRS complex tachycardia (ventricular rate >150) who is unstable (eg, chest pain, pulmonary edema, lightheadedness, hypotension) should be immediately treated with synchronized electrical cardioversion.
Synchronized electrical cardioversion may also be used to treat stable VT that does not respond to a trial of intravenous medications. It is also recommended for the treatment of the following:
- Supraventricular tachycardia due to reentry
- Atrial fibrillation
- Atrial flutter
- Atrial tachycardia
- Monomorphic VT with pulses
Contraindication:
Contraindications include known digitalis toxicity–associated tachycardia, sinus tachycardia caused by various clinical conditions, and multifocal atrial tachycardia.
In addition, because patients with atrial fibrillation are at risk for developing thrombi in the left atrium appendage, predisposing them to increased stroke risk, patients who are not anticoagulated should not undergo cardioversion without a transesophageal echo that can assess the presence of a left atrial thrombus.
Synchronized cardioversion should also not be used to treat VF since the cardioverter may not sense a QRS wave and may, therefore, fail to deliver a shock. Synchronized cardioversion is also not appropriate for the treatment of pulseless VT or polymorphic (irregular) VT since these require high-energy, unsynchronized shocks (ie, defibrillation doses). In addition, cardioversion is not effective for the treatment of junctional tachycardia.
(Unstable polymorphic (irregular) VT with or without pulses is treated as VF using unsynchronized high-energy shocks ie, defibrillation doses)
Procedure to cardiovert:
- ACLS guidelines should be followed as indicated. The key components in preparing the patient are intravenous access, airway management equipment, sedative drugs, and a cardioverter/defibrillator monitoring device.
- The patient should be adequately sedated with a short-acting agent such as midazolam or propofol (may need an anaesthetist intervention). In addition, an opioid analgesic, such as fentanyl, is commonly used. Reversal agents, such as flumazenil and naloxone, should be available.
- The defibrillator should be placed in the synchronized mode, which permits a search for a large R or S wave. Manual Sync button depression by the operator causes the defibrillator to discharge an electric current that lasts less than 4 milliseconds and avoids the vulnerable period of cardiac repolarization where VF can be induced. The operator should be aware of this brief delay as the cardioverter searches for a large positive or negative deflection. If deflections are too small for the defibrillator to synchronize, the physician can change the leads or place them closer to the patient's chest or heart. If the patient develops VF, always turn off synchronization to avoid delay in energy delivery.
Pads placements:
Two options exist for the placement of pads on the chest wall:
- If the patient's size permits, the first is placed in the anterolateral position in which a single pad is placed on the left fourth or fifth intercostal space on the midaxillary line; the other pad is placed just to the right of the sternal edge on the second or third intercostal space.
- The second option is the anteroposterior position. A single pad is placed to the right of the sternum, as above, and the other pad is placed between the tip of the left scapula and the spine.
Although there is a risk of receiving a shock if touching the patient or the stretcher, bed, or other equipment in which the patient is in contact, there has been recent evidence that continued contact with the patient is safe during biphasic defibrillation. Pacemakers and ICDs should be at least 10 cm from direct contact with paddles and should eventually be interrogated for any malfunction after cardioversion. The anteroposterior approach is preferred in patients with implantable devices to avoid shunting current to the implantable device and damaging the system.
Energy requirements:
For electric cardioversion in children, the recommended starting energy dose is 0.5 to 1 J/kg. If that fails, increase the dose up to 2 J/kg