Clinical Practice Case 9
 Case 9
Case 9
You are seeing a 6-week-old infant who was brought to the emergency department because the mother noted breathing difficulty, poor feeding, and vomiting today.
General Assessment
You see an obviously tachypneic infant with occasional grunting respirations who appears irritable and is not consoled by her mother. Her colour appears mottled and greyish.
9A
Based on your general assessment, what is your impression of this infant's condition?
You should be very worried about this infant's appearance. She has respiratory distress with grunting respirations and mottled colour with irritability. This clinical picture suggests lung tissue disease, which is often complicated by hypoxemia.
9B
Does the child need immediate intervention? If so, what intervention is indicated?
The child is in severe respiratory distress. Your first actions are to call for additional help so that you can quickly place the infant on high-flow oxygen, a cardiac monitor and pulse oximeter, and establish vascular access. The infant has good respiratory effort, so there is no obvious need to provide ventilatory support at this time.
Primary Assessment
After you provide oxygen and place the infant on a monitor, the infant appears to be breathing adequately, so you proceed with your primary assessment.
The pulse rate displayed by the pulse oximeter is 275/min with Sp02 of 99% on a high-flow oxygen delivery system. Blood pressure is 72/55 mm Hg.
Auscultation of the lungs reveals bilateral scattered crackles at the lung bases with fair air entry. Occasional grunting respirations are still heard. You hear a very fast, regular rhythm; the rate is so fast you are unable to tell if there is a murmur. You do not hear a gallop rhythm.
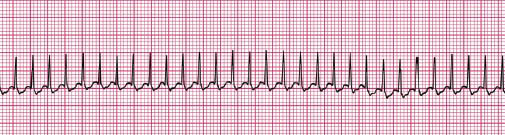
The infant has weak central pulses, and you cannot feel definite peripheral pulses. The extremities are cool, with a capillary refill of at least 5 seconds. The infant remains fussy with good muscle tone and vigorous crying. The skin appears less mottled with oxygen administration. The rhythm on the monitor is seen below:
9C
How do you categorize this infant's condition now?
This infant has a tachycardia (>200/min) with poor perfusion.
9D
Is this a narrow-complex or wide-complex rhythm? Why is that distinction important?
Since the heart rate is well in excess of 200/min and the history does not suggest a cause for shock producing tachycardia (ie, a sinus tachycardia), this is most likely a supraventricular tachycardia (SVT). Once you see a fast rhythm on the monitor, your next decision is to determine if the rhythm is narrow or wide.
A narrow rhythm (≤.08 sec) is supraventricular, whereas a wide rhythm (>0.08 sec) may be either a supraventricular rhythm with aberrant conduction or ventricular tachycardia (VT). Since this discrimination is often difficult, you should treat wide-complex tachycardia as VT unless the child is known to have aberrant conduction. When the patient is poorly perfused with a wide-complex tachycardia, early synchronized cardioversion is indicated. If the child has narrow-complex tachycardia, you may attempt pharmacologic conversion if IV or I0 access is readily available.
9E
What is your decision and action for this infant?
In this case, recommendations for management are based on the Algorithm for Pediatric Tachycardia With Pulses and Poor Perfusion.
With poor perfusion, the infant will likely require synchronized cardioversion. But if you have vascular access established (or it can be readily established), you may first attempt to convert the rhythm with a dose of adenosine, using 0.1 mg/kg (maximum first dose 6 mg) by rapid IV infusion. You may also attempt to convert the rhythm with a vagal maneuver by placing iced water in a bag or glove on the infant's face (without obstructing the infant's nose), provided the vagal maneuvers do not delay pharmacologic or electrical cardioversion.
This infant is irritable and fairly vigorous despite the poor perfusion. In this setting, the experienced provider may consider the use of sedation prior to cardioversion. Provide sedation agents cautiously using a small dose of a benzodiazepine (midazolam, 0.05 mg/kg is a reasonable choice) to provide sedation for the shock
9F
What would be your action(s) if the infant had readily palpable distal pulses with this rhythm?
The presence of good pulses indicates that this infant has adequate perfusion and does not need immediate cardioversion. Instead, you may attempt vagal maneuvers and adenosine after IV/IO access is established. In addition, you should seek consultation with a pediatric cardiologist or other knowledgeable providers to help with management.
Case Progression
A high-flow oxygen delivery system is continued, and the infant has an IV cannula inserted. The infant remains irritable and agitated.
9G
What should you do now and why?
Since the infant has vascular access available, giving a dose of adenosine (0.1 mg/kg) is reasonable. Remember that this drug requires a 2-syringe method of rapid administration. A 3-way stopcock is often used so that the drug can be given quickly and followed immediately by a flush of isotonic saline to help deliver the drug to the central circulation. If the initial dose is not effective, you can double the dose and give that dose once.

Case Progression
The infant's heart rate transiently decreased with the dose of adenosine but then went back up to 275/min again. A second (larger) adenosine dose was also ineffective, so after a small dose of midazolam, you provide synchronized cardioversion at a dose of 0.5 J/kg.
Following the shock, the monitor shows the rhythm seen below at a rate of about 165/min. On reassessment, the infant continues to have tachypnea with some grunting. Colour is improved and Sp02 is 100%. Blood pressure is 82/58 mm Hg. Pulses can now be felt distally but are weak. Central pulses are improved.

9H
How do you categorize this infant's condition now?
The infant has improved perfusion following successful cardioversion to a sinus rhythm. The infant still has evidence of lung tissue disease, which is likely secondary to pulmonary edema from congestive heart failure induced by the tachycardia.
9I
What are your actions now?
At this time the best approach is often careful observation rather than administration of a vasoactive drug. Recall that SVT may be induced by catecholamines, so giving a catecholamine may reinitiate the SVT. You should obtain an ECG to analyze the rhythm. The experienced provider may look for the presence of delta waves or other abnormalities. In addition, if not already obtained, consultation with a pediatric cardiologist is indicated.
9J
What are other causes of narrow-complex tachycardia?
The initial decision making (differential diagnosis) of the causes of a narrow-complex tachycardia is between SVT versus sinus tachycardia.
The child with sinus tachycardia typically has a history compatible with a cause of the tachycardia, such as shock, sepsis, a high fever, or vomiting and diarrhea leading to serious dehydration.
SVT is typically associated with an extra conduction pathway for impulse conduction in the heart. Other cardiac causes of narrow-complex tachycardia include atrial flutter and atrial fibrillation, but these are uncommon rhythms in infants unless they have underlying congenital heart disease.
9K
What are causes of wide-complex tachycardia in infants and children?
As previously noted, wide-complex tachycardia may result from aberrant conduction of an SVT, but you should treat a wide-complex tachycardia as VT unless the child is known to have aberrant conduction.
Wide-complex tachycardia is a relatively uncommon rhythm in children, but it can be seen in children with cardiomyopathy, myocarditis, congenital heart disease, drug ingestions (particularly tricyclic antidepressants), and electrolyte disturbance, particularly hyperkalemia.
In children with abnormal heart function or anatomy from any of the reasons noted above, hypomagnesemia or hypocalcemia may predispose to the development of VT.
Case Conclusion
You consult a pediatric cardiologist. The infant is admitted to the pediatric ICU for careful monitoring. An arterial blood gas is obtained, and it shows that the infant had mild metabolic acidosis. Once the blood pressure is stabilized and perfusion is improved, you give the infant a dose of Lasix. The infant has a good urine output response and improved respiratory examination within a few hours. The pediatric cardiologist recommends that you administer propranolol (a Beta blocker). This infant had supraventricular tachycardia, most likely from an accessory pathway in the heart.




