Self Assessment ECG
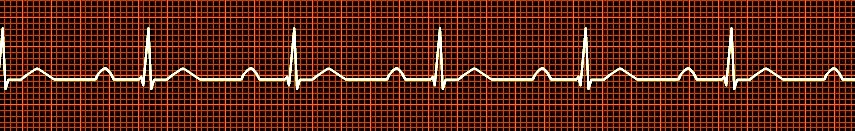
Non shockable
Sinus rhythm with First Degree Block

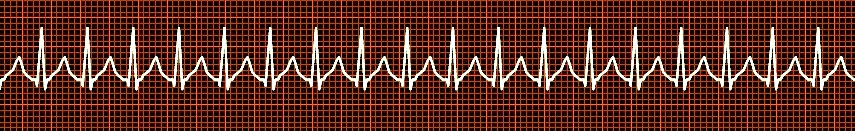
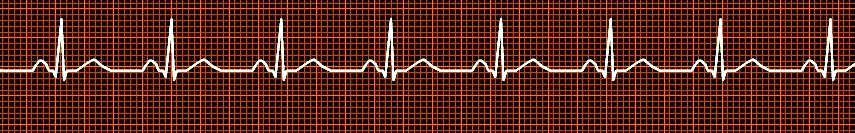
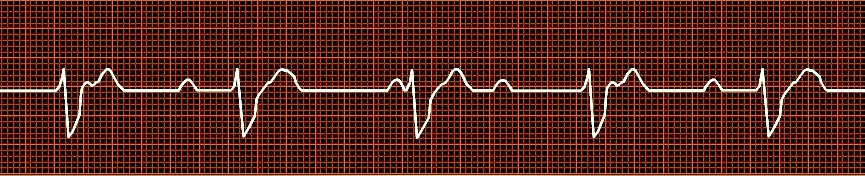
Atrial Fibrillation
Non Shockable (Defibrillation), but can be cardioverted with a synchronized shock
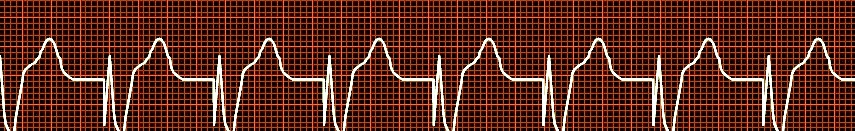
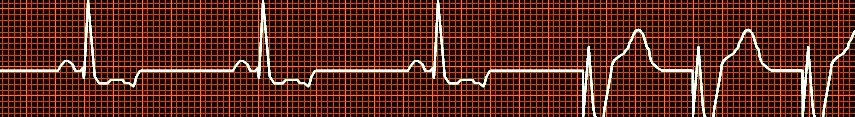
Atrial Fibrillation
Atrial frequency of > 300/min with absolute arrhythmia and a ventricular rate of > 90 beats/min (see also atrial fibrillation with slow ventricular response, ).
ECG: Absence of P waves, irregular isoelectric line. The QRS complexes are usually narrow. If a wide QRS complex is present, the following differential diagnoses have to be considered:
- existing bundle branch block
- aberrant conduction through the AV node
- atrial fibrillation in a WPW syndrome ( >> ). Caution: Aberrant conduction with broad ventricular complexes is often misinterpreted as ventricular runs. Sometimes atrial fibrillation waves are easy, and sometimes very hard, to diagnose. The irregular rate of the ventricular complexes help make the diagnosis.
Treatment
A protocol is usually followed:.
1. Heart rate control: In "fast" atrial fibrillation, rate control is most important. This is accomplished by digitalis, calcium channel blockers (verapamil) and betablockers. Both digitalis and calcium channel blockers are contraindicated for WPW syndrome with atrial fibrillation
2. Anticoagulation: According to the textbooks, patients with atrial fibrillation existing for more than three days should be anticoagulated with heparin or warfarin for three weeks before attempting conversion. In some cases , a t ransesophageal echocardiography ( TEE), providing a high quality picture of the atria, is suitable for excluding a left atrial thrombus so that cardioversion may be performed immediately.
After successful cardioversion, anticoagulation therapy must be continued for 4 - 6 weeks, since atrial contraction is still compromised despite the sinus rhythm. If conversion to a sinus rhythm remains unsuccessful, long-term anticoagulation therapy is necessary. Patients with a high embolic risk receive high dose warfarin, while those with a smaller risk with heart disease receive low dose warfarin therapy or 300 mg of aspirin a day.
Idiopathic atrial fibrillation (" lone atrial fibrillation") with a normal left atrium does not require anticoagulation in patients < 60 years, while 300 mg of aspirin/day are recommended for older patients.
Supravintricular Tachycaria - Non shockable
A Reentrant tachycardia arising from the AV-node.
Epidemiology: Reentry is Common form of supraventricular tachycardia, most common cause of paroxysmal supraventricular tachycardia ( PSVT) more common in women.
Pathophysiology: A tachycardia occurs when an impulse deviates into a circular conduction pathway, forming a loop. In typical AV reentry, the impulse runs through a slow pathway first and backwards through a fast pathway in the AV node. In an atypical AV reentry, the depolarization wave runs the other way around.
ECG: Narrow QRS complexes. The P waves are hidden in the QRS complex and are usually not visible in a standard ECG (sometimes in the early ST segment and the QRS complex). An AV reentry can lead to repolarization disturbances and ST depression.
Treatment: Good response to verapamil and adenosine IV. If the AV reentry is chronic, vagal maneuvers such as a carotid sinus massage or swallowing ice water can be attempted. If still unsuccessful, drugs like verapamil or antiarrhythmics can be used. Curative treatment is possible through a catheter ablation of the slow conduction pathway (pacemaker only necessary in rare cases) or the fast conduction pathway (pacemaker frequently necessary).
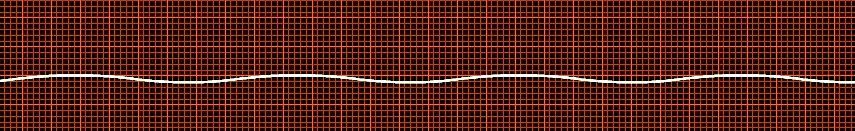
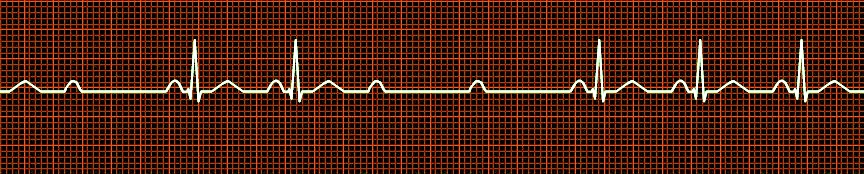
Non Shockable rhythm
Asystole
No electrical activity from the myocardium. It indicates severe hypoxic heart.
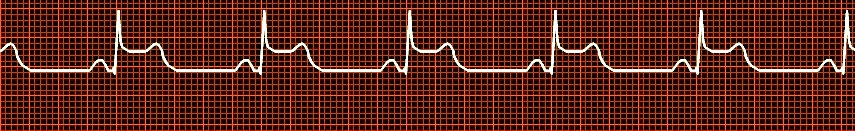
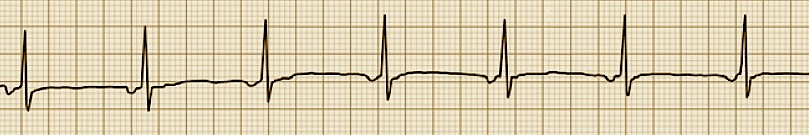
Non shockable rhythm
Sinus Bradycardia with ST elevation
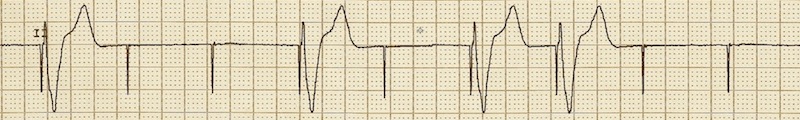
Ventricular Tachycardia - If no pulse, then it is shockable
Tachycardia originating from a ventricular focus and lasting > 30 s.
ECG:
Broad QRS complexes at a rate of > 90 beats/min. The ventricular ectopic beats can be of a single morphology ( uniform ventricular tachycardia), or of different morphologies ( multiform ventricular tachycardias), or of c hanging polarity ( torsade de pointes, frequently induced by antiarrhythmic drugs).
Caution:
Ventricular tachycardias are always a life threatening complication and require observation and treatment in a coronary care unit!
Normal Sinus rhythm
Non Shockable rhythm
Non Shockable rhythm
Second Degree Block: Mobitz Type II
Definition:
Intermittent failure of the AV conduction, the PR interval remains within normal limits.
ECG:
Intermittent drop of a ventricular complex. The PR interval is constant and within normal limits. The underlying event is the prolongation of the HV interval.
Prognosis:
Frequent progression to third degree AV block.
Non shockable rhythm
junctional escape rhythm, which has a depolarization rate of 50-60 beats/min
Definition:
Complete block (Third Degree) of the AV conduction. A Non shockable rhythm.
ECG:
Atria and ventricles beat independently, with no relation between P waves and QRS complexes. There is no AV conduction; the ventricular depolarization is paced by an escape mechanism, which can be localized in the bundle of His (small QRS complex), or in the ventricle (BBB-like ventricular complex). Failure of the ventricular escape rhythm can lead to an asystole ( Adams-Stokes attack)
still showing regular P waves.
Causes:
A third-degree AV block occurs as a complication of posterior myocardial infarction (occlusion of the artery supplying the AV node) and in bacterial endocarditis
Treatment:
Third degree AV block is an absolute indication for pacemaker placement except in an old AV block with a stable escape rhythm.
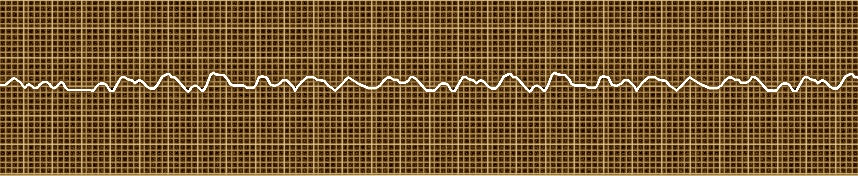
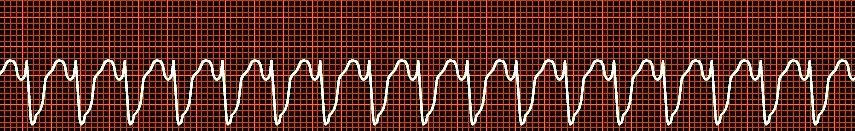
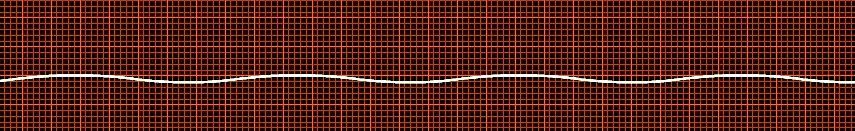
A shockable rhythm
VF
Definition:
Chaotic ventricular e lectrical discharge from multiple reentry loops resulting in hemodynamic collapse
Cause:
The most common cause of ventricular fibrillation (VF) is acute ischemia resulting from myocardial infarction . The most common causes of sudden cardiac death are fast ventricular tachycardias and ventricular fibrillation.
Prognosis:
Patients who have survived episodes of ventricular fibrillation should be treated in a coronary care unit even in the absence of myocardial infarction. The predictive value of controlled ventricular stimulation is less than in monomorphic tachycardias.
Treatment:
In acute VF, emergency therapy is electrical defibrillation. In chronic VF, an implantable automatic defibrillator may be necessary
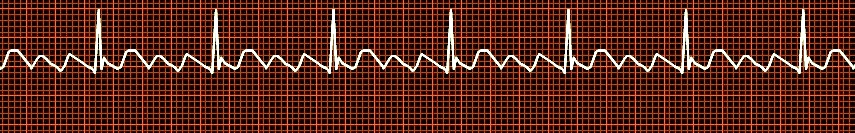
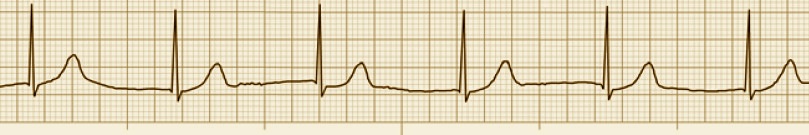
Atrial Flutter
Atrial frequency of 240-300 beats/min.
ECG Sawtooth-like P waves with regular or irregular ventricular conduction through the AV node.
A 2:1 conduction may be mistaken for a sinus tachycardia.
Diagnosis:
In the case of a 2:1 conduction, a carotid sinus massage may be helpful in makingIn the diagnosis. Due to the delayed ventricular conduction, the sawtooth-like pattern of the P waves becomes evident. If a carotid sinus massage remains ineffective, adenosine 6-12 mg IV can be administered
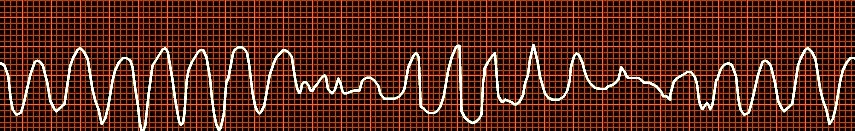
Torsades de pointes, or simply torsades is a French term that literally means "twisting of the points". It was first described by Dessertenne in 1966 and refers to a specific, rare variety of ventricular tachycardia that exhibits distinct characteristics on the electrocardiogram (ECG).
It is due to abnormal prolongation of the corrected QT interval (QTc) predisposing to malignant cardiac arrhythmias ).
The prolongation of the QT interval is a sign of repolarization disorders which predispose to arrhythmias. Primary long QT syndromes are congenital ( Jervell-Lange-Nielsen syndrome without deafness, Romano-Ward syndrome with deafness). A family history of sudden cardiac death and syncope is typical. Secondary long QT syndromes occur with antiarrhythmic drugs.
Diagnosis: The prolongation of the QT interval can be calculated using a nomogram or the Bazett´s formula.
Treatment: Primary long QT syndromes can be treated with high dose betablockers, by modification of the autonomic innervation of the heart through surgical procedure or symptomatically with an implantable defibrillator. Most importantly, in a secondary proarrhythmia, all causative agents must be discontinued.
Ventricular pacing with 100% capture.
Ventricular pacing with failure to 100% capture.
Treatment: Increase output current

Delta wave as seen in Wolf Parkinson White syndrome. (WPW)
The WPW syndrome is a congenital syndrome with premature depolarization ( preexcitation) of the ventricles through accessory AV conduction pathways.
Pathophysiology: An accessory muscular bundle, the Kent bundle, conducts the electrical impulse from the atria to the ventricles. Depolarization through the Kent bundle reaches the ventricles faster than the one leading through the AV node or the bundle of His, so that some parts of the ventricle get depolarized earlier
Junctional Rhythm
Asystole
Sinus bradycardia with ST segment depression-Pacing




