Clinical Practice Case 2
 Case 2
Case 2
You are an advanced EMS provider called to the home of a 7-year-old with breathing difficulty. Her mother says the child has had a cold for the last 2 days with increasing coughing. She is now having trouble catching her breath.
General assessment
You see a thin child who is sitting upright and using her accessory muscles. She appears worried and alertly watches you approach her. She is working hard to breathe with increased inspiratory and expiratory effort. She appears to be forcing the air out during exhalation, which appears prolonged. Her colour appears somewhat pale.
2 A
1- What is your initial impression of the child's condition and your general assessment?
2- Does the child need immediate intervention? If so, what intervention is indicated?
1- The initial appearance is worrisome in view of the child's anxiety and labored breathing with prolonged, forced expiratory effort. The child is still alert, which suggests she is not in respiratory failure, but you should be worried by the child's general assessment.
2- Essentially you should give oxygen to all children with significant respiratory effort and distress while you rapidly proceed to your primary assessment.
2 B
What is the significance of the prolonged, forced expiratory effort?
The prolonged, forced expiratory effort and the significance of the child's overall respiratory effort are the most striking elements of the child's physical examination. The presence of prolonged, forced exhalation strongly suggests that the child has lower airway obstruction. When the lower airway obstruction is severe, as seen in this child, an increase in both inspiratory and expiratory effort is required to overcome the small airway obstruction. An increased effort throughout the breathing cycle is always more worrisome than an isolated increase in expiratory effort.
Primary Assessment
As you talk to the patient and ask questions, you note that she is unable to say more than one word at a time. She has marked intercostal and suprasternal retractions during inspiration with a forced, prolonged expiratory phase and occasional grunting. By auscultation, air entry is markedly decreased over her distal lung fields, and you hear high-pitched wheezing centrally throughout exhalation. Her heart rate is 144/min. Respiratory rate is 24/min. Her heart sounds are normal although they sound somewhat distant. Her pulses are weak distally.
You note that her radial pulse disappears and reappears in a somewhat rhythmic manner every few heartbeats in association with her breathing; her pulse disappears during inspiration and reappears with exhalation. Her distal extremities are cool with a capillary refill of approximately 2 seconds. She is alert with good muscle tone. No rash is noted. Her blood pressure is 126/78 mm Hg. The pulse oximeter is not consistently reading, but when it does show a value, the displayed Sp02 is 84% to 88%.
2 C
1- What is your categorization of the child's condition based on the primary assessment?
2- Based on your current impression, does the child need immediate intervention now?
3- If so, what intervention is indicated?
1- This child has marked respiratory distress due to lower airway obstruction. The inability to speak using more than one word at a time is very worrisome and confirms that this child's tidal volume is limited.
2- This child requires urgent therapy to improve oxygenation.
3- Administer oxygen while directly treating the cause of the lower airway obstruction. In children, the initial specific treatment is typically nebulized albuterol therapy combined with corticosteroid therapy. Parenteral corticosteroids are indicated only in children with severe distress who cannot safely take oral therapy (eg, oral therapy is commonly used in the ED). Given this child's severe distress, if medical control or protocol allows, IV administration of corticosteroids would be reasonable. Once the child arrives in the ED, inhaled ipratropium bromide should be used in children with severe asthma. See Chapter 2: Management of Respiratory Distress and Failure in the PALS Provider Manual and Pharmacology on the student CD for more details on medications for the treatment of asthma.
2 D
What conditions are associated with wheezing and a prolonged, forced expiratory phase in infants and children?
In infants wheezing and a prolonged expiratory effort is most commonly seen with bronchiolitis, a viral infection of the small airways. In older children, these signs are most commonly seen in association with asthma.
2 E
1- What is the significance of the variability in radial pulse volume in this patient?
2- Why does this variability occur?
1- The variability in this child's palpable pulse volume is a sign of pulsus paradoxus. Note that this pulse volume variation may result in inaccurate pulse oximetry readings.
2- Severe air trapping in the lower airways causes hyperinflation. With each inspiratory effort, the heart is squeezed by the overinflated lungs and by the pericardium. The pericardial compression develops because the pericardium attaches to the diaphragm, and the diaphragm is flattened in patients with severe asthma. Each time the patient breathes in, the diaphragm moves downward. This adds additional tension to the pericardium and impedes filling of the heart. Thus stroke volume is decreased during inspiration, resulting in pulsus paradoxus. See the Figure.
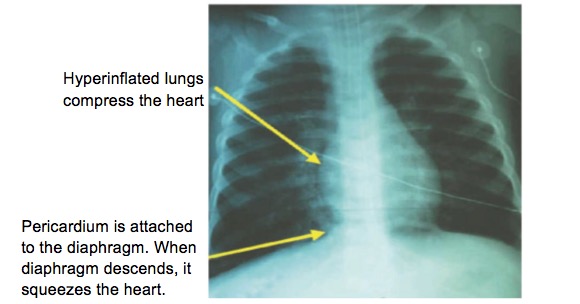
Figure 1. Chest x-ray of a child with asthma illustrates the relationship between the lungs and heart. As the lung volume increases, the heart is compressed. In addition, the parietal pericardium is attached to the diaphragm. As the child inhales, the diaphragm flattens further and pulls the pericardium more tightly around the heart. Both of these actions impede venous return and thus impair stroke volume during inspiration, leading to the pulsus paradoxus.
Case progression
While allowing the child to remain in the position most comfortable for her, you provide high-flow oxygen using a face mask and begin a nebulizer treatment with 2.5 mg of albuterol. In response to these interventions her Sp02 increases to 95% to 98%. You place ECG leads for monitoring and reassess the child's respiratory effort. You obtain additional history using the SAMPLE mnemonic.
2 F
1- What are the elements of the SAMPLE mnemonic?
2- What specific history questions are you interested in knowing about this child?
1-
Signs and symptoms
Allergies
Medications
Past medical history
bast meal
Events leading to presentation
2- The answers to the SAMPLE mnemonic questions for this child include the following:
- Signs and symptoms began 2 days ago with a cold that progressed to more coughing today. At times the child's coughing resulted in emesis, and she has not been able to take much orally.
- She has a history of allergic rhinitis but no other allergies.
- The only medications her mother gave was a cough syrup, which has not helped.
- Her Past medical history is notable for a history of coughing with previous colds, but she has never been this ill before. She also coughs frequently at night and has complained of tightness in her chest and coughing after she runs.
- Her last oral intake was several hours ago.
- There was no event leading to this illness other than the recent cold.
2 G
The child has clinically improved in response to your interventions.What are your treatment priorities now?
You need to maintain vigilance, however, since her respiratory distress may worsen as the initial effects of the albuterol treatment fade. You should monitor and reexamine the child frequently during transport to the emergency department. Ideally, continuous pulse oximetry should be maintained during transport.
Case conclusion
You continue high-flow oxygen administration and repeat a nebulized albuterol treatment during transport to the emergency department. Reassessment shows that the child is breathing more easily with less effort. She is now able to answer questions using several words at a time.
2 H
What other conditions cause lower airway obstruction?
In addition to asthma, viral or mycoplasma infection may cause inflammation of the small airways. In infants this presents as bronchiolitis, with respiratory syncytial virus (RSV) being the most common cause. In older children (~5 years) mycoplasma is the most common cause of wheezing-associated lower respiratory tract infection. Inhalation injury and anaphylaxis may also cause bronchospasm, leading to wheezing and signs of lower airway obstruction.
 Summing up
Summing up
This child had acute, severe asthma requiring urgent therapy. She was at significant risk of deterioration in view of the clinical evidence for severe lower airway obstruction manifested by her inability to speak more than one word at a time and the significant pulsus paradoxus detected by simple palpation of her pulse. If respiratory failure develops, remember that effective bag-mask ventilation may require the use of a 2-person bag-mask ventilation approach: 1 rescuer performs a head tilt-chin lift and seals the mask to the face while the 2nd rescuer compresses the ventilation bag. Avoid rapid ventilation rates since air trapping and further impairment of cardiac output will occur with overventilation.
The treatment of lower airway obstruction from asthma typically consists of bronchodilator therapy (nebulized albuterol and ipratropium bromide and intravenous (IV) magnesium in severe cases) along with systemic corticosteroid therapy. When lower airway obstruction is caused by a viral infection (eg, RSV bronchiolitis), treatment is largely supportive with oxygen. Nebulized albuterol or epinephrine may be helpful. The role of steroids in bronchiolitis remains controversial.
In more severe cases of asthma or bronchiolitis, positive airway pressure support in the form of CPAP in infants or BiPAP in children may be helpful and may reduce the need for mechanical ventilation.




