Acute Coronary Syndrome (ACS)
A condition that causes a sudden imbalance between myocardial oxygen consumption and demand.
Often this is a result of a rupture of a fibrous cap of a coronary atheroma which exposes the underlying subendothelial tissue leading to thrombus formation.
Other conditions that cause this imbalance include coronary vasospasm, hypotension, anemia, hypertension, tachycardia, valvular heart disease, cardiomyopathy, myocarditis, pulmonary embolism, and sepsis

Acute Coronary Syndrome
|
Download the video file [0.0 MB] |
ACS
Acute coronary syndrome (ACS) is a spectrum of clinical presentations ranging from ST-segment elevation myocardial infarction (STEMI) to presentations found in non–ST-segment elevation myocardial infarction (NSTEMI) or in unstable angina. It is almost always associated with rupture of an atherosclerotic plaque and partial or complete thrombosis of the infarct-related artery.
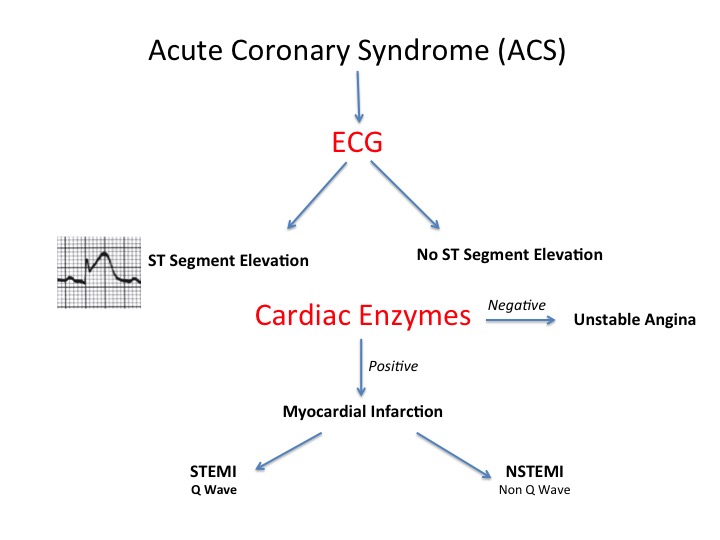
Unstable angina, non-ST-segment myocardial infarction (NSTEMI), and ST-segment myocardial infarction (STEMI) differ with regard to duration, severity, and treatments.
Unstable Angina
Cause:
• Thrombus partially or intermittently occludes the coronary artery
Signs and Symptoms:
• Pain with or without radiation to arm, neck, back, or epigastric region
• Shortness of breath, diaphoresis, nausea, lightheadedness, tachycardia, tachypnea, hypotension or hypertension, decreased arterial oxygen saturation and rhythm abnormalities
• Occurs at rest or with exertion; limits activity
Diagnostic Findings:
• ST-segment depression or T-wave inversion on electro cardiography
• Cardiac biomarkers not elevated
Management:
• Oxygen to maintain oxygen saturation level at > 94%
• Nitroglycerin or morphine to control pain
• Beta-blockers, angiotensin-converting enzyme inhibitors, statins (started on admission and continued long-term), clopidogrel, unfractionated heparin or low- molecular-weight heparin, and glycoprotein IIb / IIIa inhibitors.
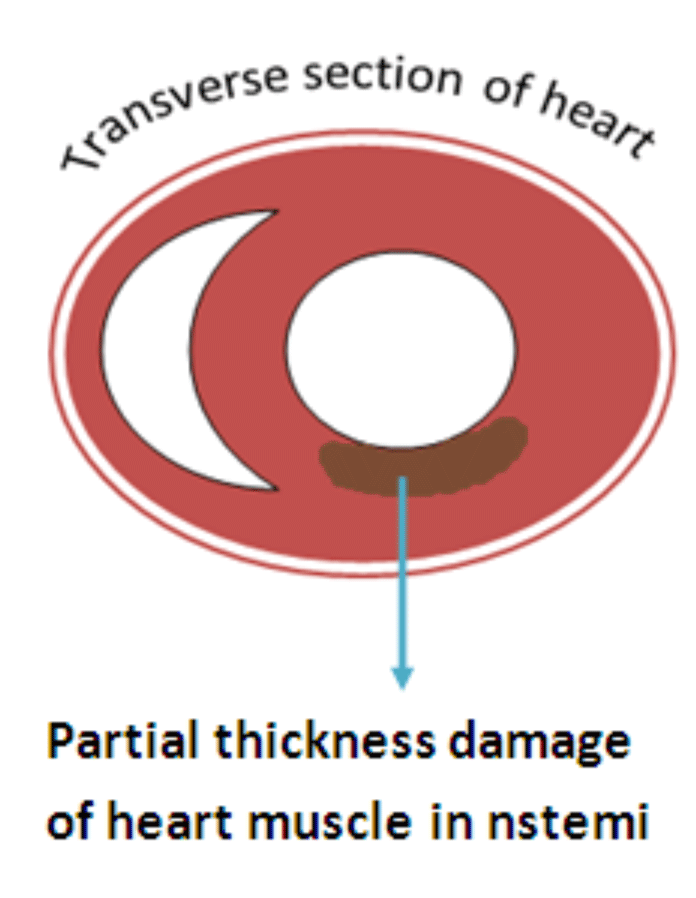
Non-ST-Segment Elevation Myocardial Infarction (NSTEMI)
Cause:
• Thrombus partially or intermittently occludes the coronary artery leading to partial wall thickness MI.
Source: http://www.medicaltechnologyinnovation.com/heartattack.php
Signs and Symptoms:
• Pain with or without radiation to arm, neck, back, or epigastric region
• Shortness of breath, diaphoresis, nausea, lightheaded ness, tachycardia, tachypnea, hypotension or hypertension, decreased arterial oxygen saturation and rhythm abnormalities
• Occurs at rest or with exertion; limits activity
• Longer in duration and more severe than in unstable angina
Diagnostic Findings:
• ST-segment depression or T-wave inversion on electro cardiography
• Cardiac biomarkers are elevated.
Management:
• Oxygen to maintain the SPO2 level at > 94%
• Nitroglycerin or morphine to control pain
• Beta-blockers, angiotensin-converting enzyme inhibitors, statins (started on admission and continued long-term), clopidogrel, unfractionated heparin or low- molecular-weight heparin, and glycoprotein IIb / IIIa inhibitors
• Cardiac catheterization and possible percutaneous coronary intervention for patients with ongoing chest pain, hemodynamic instability, or increased risk of worsening clinical condition
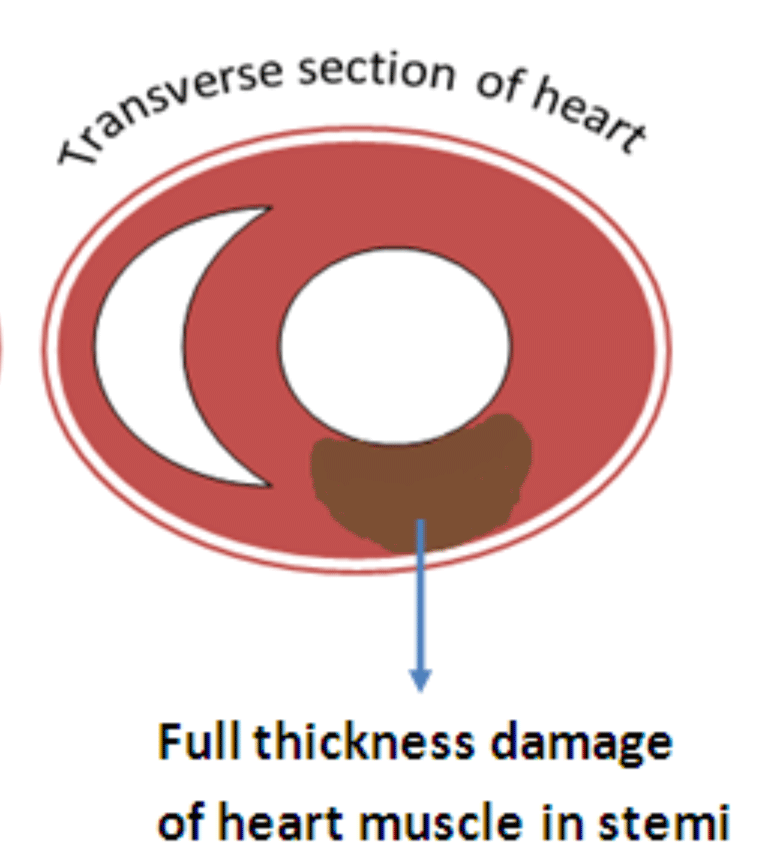
ST-Segment Elevation Myocardial Infarction (STEMI)
Cause:
• Thrombus fully occludes the coronary artery leading to full wall thickness MI.
Source: http://www.medicaltechnologyinnovation.com/heartattack.php
Signs and Symptoms:
• Pain with or without radiation to arm, neck, back, or epigastric region
• Shortness of breath, diaphoresis, nausea, light headedness, tachycardia, tachypnea, hypotention or hypertension, decreased arterial oxygen saturation and rhythm abnormali ties
• Occurs at rest or with exertion; limits activity
• Longer in duration and more severe than in unstable angina (irreversible tissue damage [infarction] occurs if perfusion is not restored)
Diagnostic Findings:
• ST-segment elevation or new left bundle branch block on electrocardiography
• Cardiac biomarkers are elevated
Management:
• Oxygen to maintain the SPO2 level at > 94%
• Nitroglycerin or morphine to control pain
• Beta-blockers, angiotensin-converting enzyme inhibitors, statins (started on admission and continued long-term), clopidogrel (Plavix), unfractionated heparin or low-molecular-weight heparin
• Percutaneous coronary intervention within 90 minutes of medical evaluation
• Fibrinolytic therapy within 30 minutes of medical evaluation.

Coronary angiography

Catheterisation Left and Right Coronary Arteries
Summary of Management
Initial therapy focuses on the following:
- Stabilising the patient’s condition
- Alleviate pain
- Antithrombotic therapy
Pharmacologic anti-ischaemic therapy includes the following:
- Nitrates (for symptomatic relief)
- Beta-blockers (eg, metoprolol): These are indicated in all patients unless contraindicated
Pharmacologic antithrombotic therapy includes the following:
- Aspirin
- Clopidogrel
- Glycoprotein IIb/IIIa receptor antagonists (abciximab, eptifibatide, tirofiban)
Pharmacologic anticoagulant therapy includes the following:
- Unfractionated heparin (UFH)
- Low-molecular-weight heparin (LMWH; dalteparin, nadroparin, enoxaparin)
- Factor Xa inhibitors (rivaroxaban, fondaparinux)
Additional therapeutic measures that may be indicated include the following:
- Thrombolysis
- Percutaneous coronary intervention (preferred treatment for ST-elevation MI)
Current guidelines for patients with moderate- or high-risk ACS include the following:
- Early invasive approach
- Concomitant antithrombotic therapy, including aspirin and clopidogrel, as well as UFH or LMWH
Initial Drug Therapy for Acute Coronary Syndrome (ACS)
Drug Therapy | Dosing* | Considerations |
Aspirin | 162-325 mg orally, crushed or chewed; then 81-325 mg daily | Contraindicated in active peptic ulcer disease, hepatic disease, bleeding disorders, and aspirin allergy |
Oxygen | 2-4 L by nasal cannula | Maintain oxygen saturation at > 94% |
Nitro-glycerine | 0.3-0.4 mg sublingual tablets every 5 min (up to 3 doses) or 1-2 sublingual sprays every 5 min (up to 3 times)
| Assess for pain relief Monitor blood pressure, cease medication if systolic blood pressure < 90 or 100 mmHg |
Morphine | 2-4 mg IV push (may repeat every 5-15 min until pain controlled) | Indicated when pain not improved with nitro-glycerine |
* Dosages may vary depending on the selected drug. Anderson JL, et al. Circulation 2007;116(7):el48-e304; Gluckman TJ, et al. JAMA 2005;293(3):349-57; Hazinski MF, et al., editors. Handbook of emergency cardiovascular care for healthcare providers. Dallas: American Heart Association; 2008; Stringer KA, Lopez LM. Myocardial infarction. In: Wells BG, et al., editors. Pharmaco therapy handbook. 5th ed. New York: McGraw-Hill; 2003. p. 112-22.
| ||
Adjunctive Drug Therapy for Acute Coronary Syndrome (ACS)
Drug Therapy | Dosing* | Considerations |
Beta-blockers
| Administer oral dose within 24 hours of symptom onset and continue upon dis charge | Contraindicated when heart rate < 60 beats per minute, systolic blood pressure < 100 mmHg and in heart blocks, moderate-to-severe left ventricular failure, pulmonary oedema, acute asthma, or reactive airway disease.
Monitor for hypotension, bradycardia, signs of heart failure, hypoglycaemia, and bronchospasm |
Angiotensin-converting enzyme inhibitors
| Administer oral dose within 24 hours of symptom onset and continue upon dis charge | Assess for hypotension, decreased urine output, cough, hyperkalaemia, and renal insufficiency.
Contraindicated in renal failure, hyperkalaemia, angioedema, and pregnancy Monitor vital signs and blood glucose |
Statins
| Administer oral dose upon discharge when low-density lipoprotein cholesterol >100 mg/dL | Instruct patients to take at bedtime and limit grapefruit consumption.
Contraindicated in pregnancy
Monitor lipids, liver function, and creatine kinase levels, and assess for myopathy |
Clopidogrel (Plavix) | Administer loading dose, followed by 75 mg/day; continue on discharge preferred if PCI is not planned or is delayed | Contraindicated in active peptic ulcer disease, bleeding disorder, hepatic disease, or if coronary artery bypass graft surgery is planned within 5-7 days
Can be used in patients allergic to aspirin |
Glycoprotein IIb/IIIa inhibitors
| Abciximab (ReoPro) preferred if PCI is planned and can be performed without delay eptifibatide (Integrilin) or tirofiban (Aggrapreferredferred if PCI is not planned or is delayed | Contraindicated with active bleeding, bleeding disorder, surgery or trauma within last month, or platelets < 150,000/mm3 Monitor blood tests for anaemia and clotting disorders |
Anticoagulation agents
| Indicated for unstable angina, NSTEMI, and STEMI | Monitor complete blood count, platelets, bleeding times, blood urea nitrogen, and creatinine levels |
* Dosages may vary depending on the selected drug. Anderson JL, et al. Circulation 2007;116(7):el48-e304; Gluckman TJ, et al. JAMA 2005;293(3):349-57; Hazinski MF, et al., editors. Handbook of emergency cardiovasular care for healthcare providers. Dallas: American Heart Association; 2008; Stringer KA, Lopez LM. Myocardial infarction. In: Wells BG, et al., editors. Pharmaco therapy handbook. 5th ed. New York: McGraw-Hill; 2003. p. 112-22. | ||
Common Fibrinolytic Drugs
Drug | Weight Dependent? | Half-Life | Dosing |
Alteplase (Activase) | Yes | 4-8 min | IV bolus dose, then 90-min continuous infusion |
Reteplase (Retavase) | No | 13-16 min | Two rapid IV bolus doses of 10 units each 30 min apart |
Tenecteplase (TNKase) | Yes | 20-24 min | Single IV bolus dose |
Peacock WF, et al. Am J Emerg Med 2007;25(3):353-66. | |||

Management of Acute Coronary Syndrome
Re-vascularization of coronary arteries
Percutaneous coronary intervention (PCI), commonly known as angioplasty, is a procedure used to treat the narrowed coronary arteries of the heart found in ACS. These stenotic segments are due to the build-up of the cholesterol deposition in the vessels' wall. PCI is usually performed by interventional cardiologists in a specialised lab.
During PCI, a cardiologist inserts a deflated balloon on a catheter from the femoral artery or radial artery up to the site of narrowing of the coronary artery. X-ray imaging is used to guide the catheter threading. At the blockage, the balloon is inflated to dilate and open the stenosed portion of the artery, allowing blood to flow. A stent is usually placed at the site of the blockage to permanently maintain the patency of the arterial lumen.
Coronary artery bypass grafting (CABG) is an alternative surgical treatment. However, the coronary revascularisation by CABG is associated with risks e.g. stroke. PCI has proven to be as effective and less costly than CABG.
Source:http://en.wikipedia.org/wiki/Percutaneous_coronary_intervention

PCI

CABG
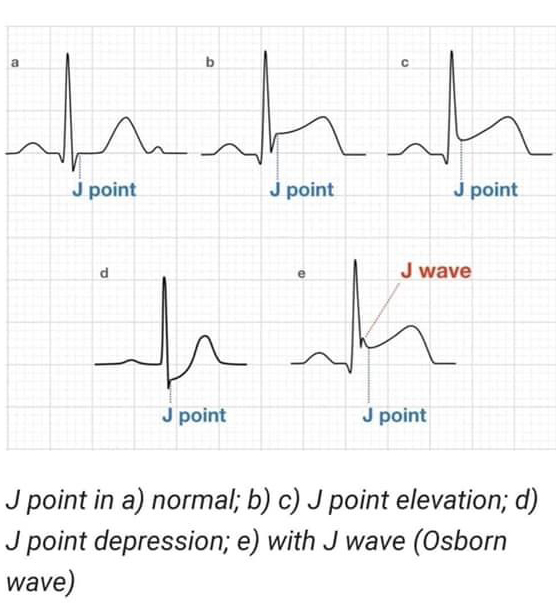
ST elevation measurement
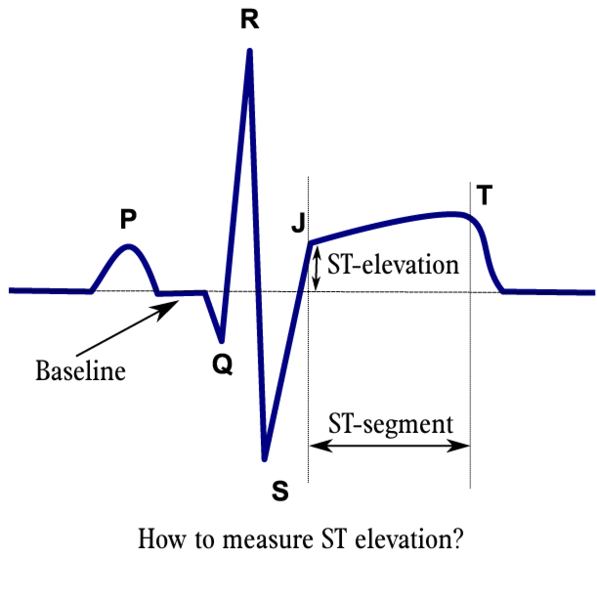 (By Rob Kreuger, medical illustrator, AMC, The Netherlands)
(By Rob Kreuger, medical illustrator, AMC, The Netherlands)
- New ST elevation at the J-point in two contiguous leads with the cut-off points: ≥0.2 mV in men or ≥ 0.15 mV in women in leads V2–V3 and/or ≥ 0.1 mV in other leads.
- (Source: http://en.ecgpedia.org/wiki/File:Stelevatie_en.png)
- What is the J point
- The J point is the the junction between the termination of the QRS complex and the beginning of the ST segment. The J (junction) point marks the end of the QRS complex
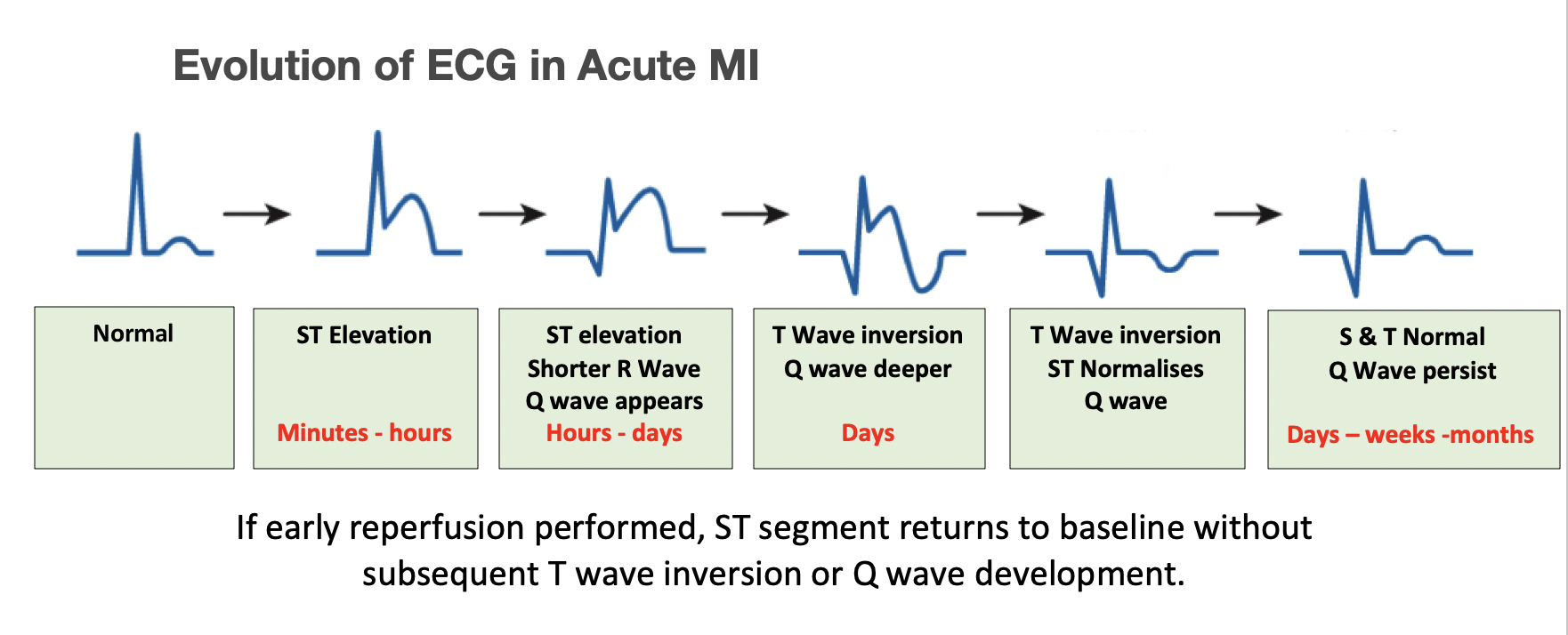
Evolution of ECG in Acute MI
Contiguous leads
What do we mean when we say leads are “contiguous”?
Contiguous leads are “next” to one another anatomically speaking. They view the same general area of the heart (specifically the left ventricle).
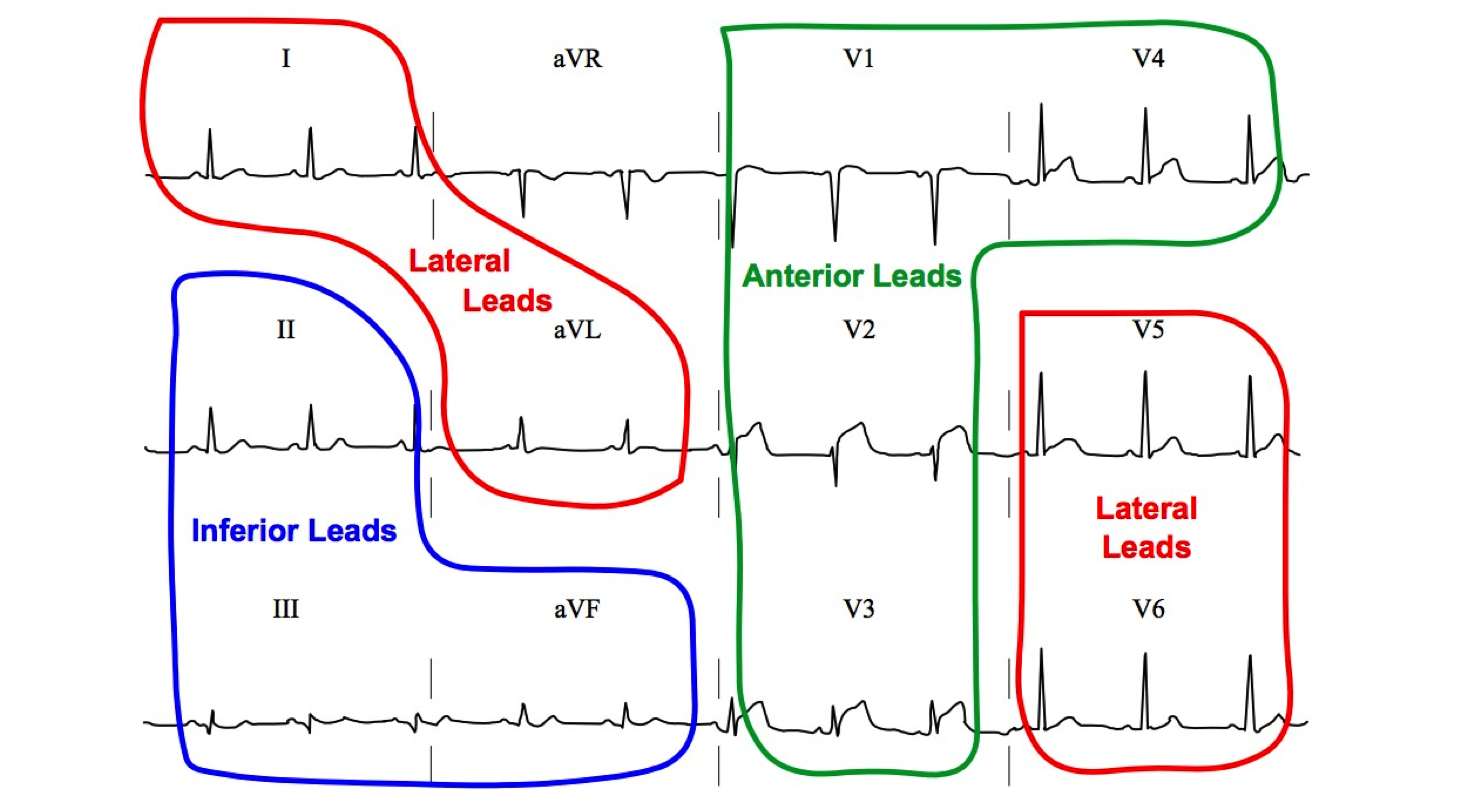
Contiguous leads in matching colours
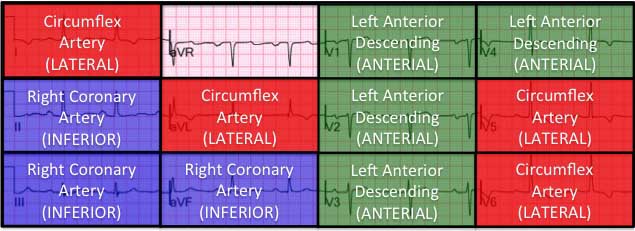
Coronary arteries
The two main coronary arteries are the left main and right coronary arteries.
Left main coronary artery (LMCA). The left main coronary artery supplies blood to the left side of the heart muscle (the left ventricle and left atrium). The left main coronary divides into branches:
The left anterior descending artery, which branches off the left coronary artery and supplies blood to the front of the left side of the heart.
The circumflex artery, which branches off the left coronary artery and encircles the heart muscle. This artery supplies blood to the outer side and back of the heart.
Right coronary artery (RCA). The right coronary artery supplies blood to the right ventricle, the right atrium, and the SA (sinoatrial) and AV (atrioventricular) nodes, which regular the heart rhythm. The right coronary artery divides into smaller branches, including the right posterior descending artery and the acute marginal artery.
The coronary arteries are classified as "end circulation", since they represent the only source of blood supply to the myocardium; there is very little redundant blood supply, which is why blockage of these vessels can be so critical.
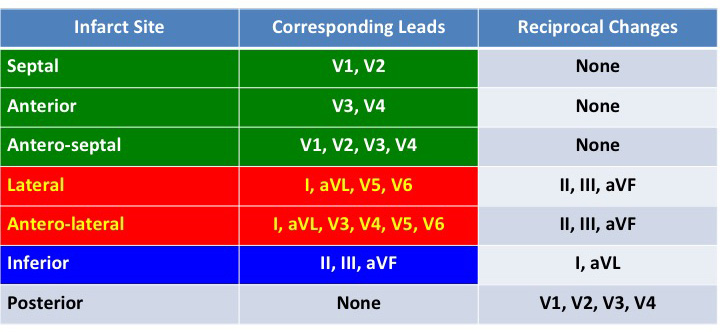
Reciprocal Changes
What do we mean by "a lead is reciprocal"?
During an acute STEMI, when ST-segment elevation is present in leads that face the acute injury, ST-segment depression will often be present in leads that face the “ischaemic boundary”.
Most acute STEMIs are documented in the distribution of the right coronary artery or the left anterior descending.
In other words, the standard 12 lead ECG poorly examine the lateral and posterior walls of the left ventricle, so there is a possibility of missing STEMI in the distribution of the circumflex artery.
That’s the main reason it is so important to carefully analyse the right precordial leads (V1R-V3R) for reciprocal changes that may indicate posterior STEMI. You can also consider using the modified leads V7, V8 and V9 to increase the sensitivity.
(Source: https://eu.nihonkohden.com/en/innovativetechnologies/syneci/whatissynthesizedecg.html)
The 12 Lead ECG provides a fairly good electrical representation of the left side of the heart. However, the right side of the heart is to some extend inadequately represented. If the 12 Lead reveals any pathological changes to the inferior aspect of the heart, an additional three 3 leads views may be added (V7, V8 & V9) to map out the right lateral and posterior views. The resulting 18 lead ECG provides a more comprehensive view picture of the heart.
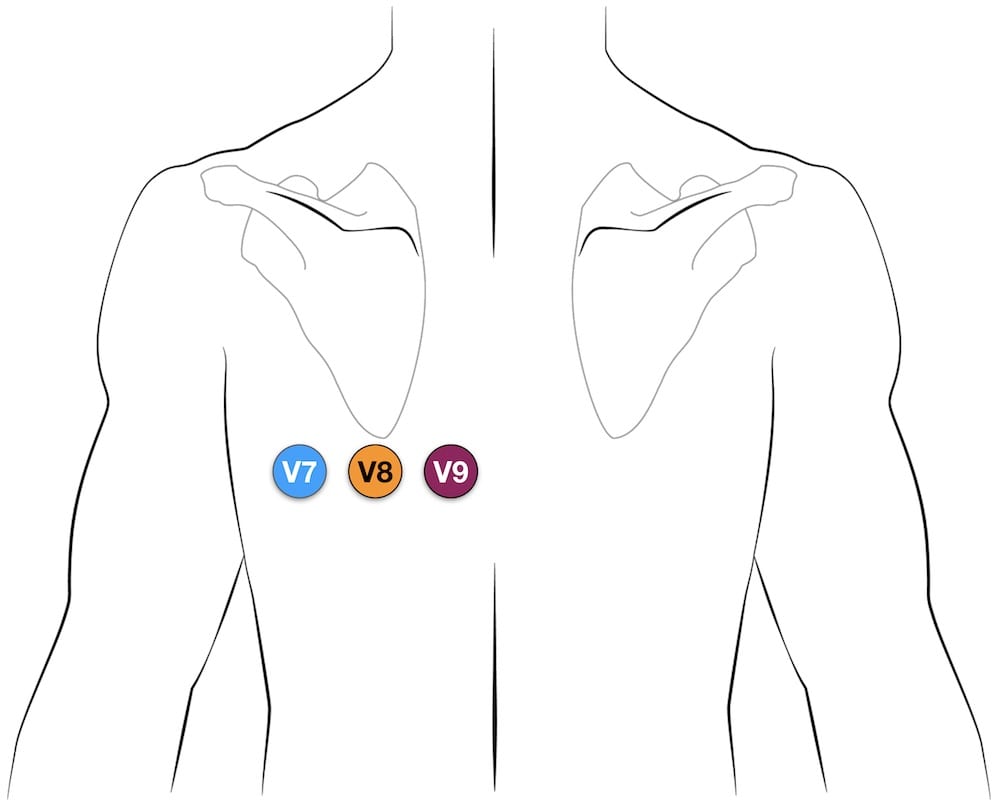
- V7 – Left posterior axillary line, in the same horizontal plane as V6.
- V8 – Tip of the left scapula, in the same horizontal plane as V6.
- V9 – Left paraspinal region, in the same horizontal plane as V6.
Source:https://litfl.com/ecg-lead-positioning/




