ECG Self Assessment Advanced (optional)
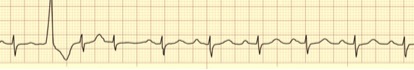
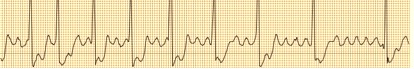
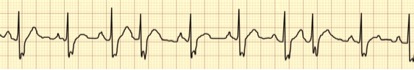
1.

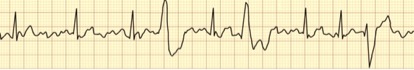
This ECG rhythm is:
a) Sinus rhythm with a run of ventricular tachycardia
b) Junctional rhythm with a run of Torsades de pointes
c) Sinus rhythm terminating in ventricular fibrillation
d) Sinus Bradycardia changing to Junctional tachycardia
to view the answer to the question aboveAnswer: a) Sinus Bradycardia changing to ventricular tachycardia
Interpretation: The ECG rhythm strip begins with a sinus rhythm: a series of narrow QRS complexes & upright P waves. A wide and premature QRS (premature ventricular complex) begins a rapid, regular series of wide QRS complexes that are most likely ventricular tachycardia. The deep Q waves might indicate a previous myocardial infarction.
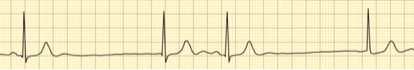
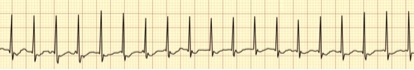
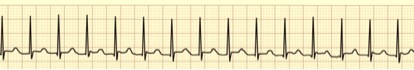
2.
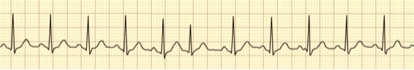
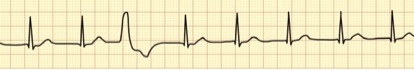
This ECG rhythm is:
a) Sinus tachycardia with a PVC
b) Atrial fibrillation with rapid ventricular response
c) Sinus tachycardia with a PAC
d) Sinus arrhythmia with a PVC
Answer: c) Sinus tachycardia with a premature atrial complex (PAC)
Interpretation: The underlying rhythm is a sinus tachycardia with narrow QRS complexes, upright P waves and a rate of about 110/minute. A premature atrial complex (PAC) is the sixth QRS present (a narrow QRS complex arriving prematurely and accompanied by a biphasic or otherwise abnormally shaped P wave - an absent or an inverted P wave suggests a PJC).
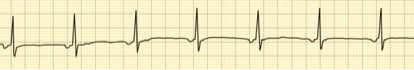
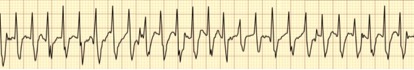
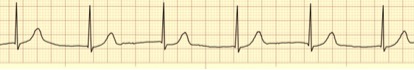
3.
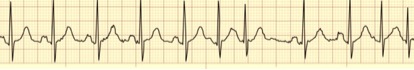
This ECG rhythm is:
a) Sinus arrhythmia
b) Atrial fibrillation with ectopic atrial beats
c) Sinus tachycardia with ventricular couplets
d) Sinus rhythm with ectopic atrial beats
Answer: d) Sinus rhythm with ectopic atrial beats
Interpretation: The underlying sinus rhythm has a rate of about 80/minute, a narrow QRS complex and upright P waves. The sinus rhythm is interrupted by ectopic atrial couplets with narrow QRS complexes. The atrial couplets have similar R-R intervals that, if sustained, would produce a rate of 166/minute.
Note: Artifact is present throughout the ECG. The presence of this degree of atrial ectopy may signify a tendency toward atrial fibrillation.
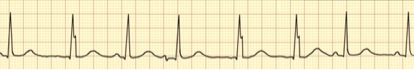
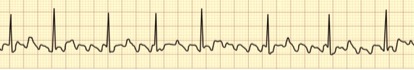
4.
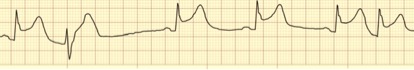
This ECG rhythm is:
a) Junctional rhythm with ST elevation and a PVC and a PAC
b) Sinus rhythm with ST elevation with a PVC and a PJC
c) Sinus Bradycardia with ST elevation with a PVC and a PJC
d) Sinus arrhythmia with ST elevation and a PVC
Answer: c) Sinus Bradycardia with ST elevation with a PVC and a PJC
Interpretation: The underlying sinus Bradycardia has a rate of about 55/minute, a narrow QRS complex, ST elevation and upright P waves. This Bradycardia is interrupted first by premature wide QRS (PVC) and later by a premature narrow QRS without any signs of a preceding upright P wave (probably a PJC).
5.
This ECG rhythm is:
a) Wandering pacemaker with a PVC
b) Sinus rhythm with a PVC and a PAC
c) Sinus tachycardia with a PVC
d) Sinus arrhythmia with a PVC
Answer: b) Sinus rhythm with a PVC and a PAC
Interpretation: The underlying sinus rhythm has a rate of about 96/minute, a narrow QRS complex, and upright P waves (albeit with a prolonged PR interval making it a first degree AV block). Premature wide QRS (PVC) interrupts the sinus rhythm early. The fourth QRS complex is narrow and premature. The preceding T wave has an upright notch suggesting a P wave with an upright component. The only reasonable option is that this is a PAC.
6.

This ECG rhythm is:
a) Sinus arrhythmia with a non-conducted PAC and a ventricular escape beat
b) Sinus Bradycardia with a non-conducted PAC and a PVC
c) Wandering pacemaker with a non-conducted PAC and a PVC
d) Sinus rhythm with a non-conducted PAC and a PVC
Answer: a) Sinus arrhythmia with a non-conducted PAC and a ventricular escape beat
Interpretation: This is rhythm requires meticulous consideration. The underlying irregular rhythm has a rate of about 70/minute, a narrow QRS complex with ST elevation and upright P waves. This is a sinus arrhythmia. The third QRS complex is wide and late, most likely a ventricular escape beat.
Note also the possible lonely P wave after the second QRS complex. While this may be a sign of second-degree AV block type II, the lonely P wave does arrive early making this a possible sign of a non-conducted PAC.
7.
This ECG rhythm is:
a) Junctional rhythm with PACs
b) Sinus rhythm with PJCs
c) Sinus Bradycardia with Junctional escape beats
d) Accelerated Junctional rhythm with PACs
Answer: c) Sinus Bradycardia with Junctional escape beats
Interpretation: The underlying sinus Bradycardia has a narrow QRS complex and upright P waves. The profoundly slow rate is somewhat rescued by late escape beats that also have narrow QRS complexes. Because the escape beats lack P waves, they originate from the AV junction.
8.

This ECG rhythm is called:
a) Sinus arrhythmia with aberrant intraventricular conduction
b) Sinus rhythm with aberrant intraventricular conduction and PACs
c) Accelerated Junctional rhythm with aberrant intraventricular conduction
d) Accelerated idioventricular rhythm with aberrant intraventricular conduction
Answer: a) Sinus arrhythmia with aberrant intraventricular conduction
Interpretation: This rhythm has a rate of close to 90/minute, a wide QRS complex and upright P waves are present before each QRS complex. While this is a sinus rhythm, its irregular pattern makes it a sinus arrhythmia.
Note: A wide QRS most often results from impulses originating in the ventricles (ventricular rhythm). In this case, though, the presence of P waves before each QRS complex strongly suggests supraventricular control (supraventricular rhythm) with aberrant intraventricular conduction.
9.
This ECG rhythm is:
a) Sinus Bradycardia
b) Ectopic atrial rhythm
c) Sinus rhythm with aberrant intraventricular conduction
d) Accelerated Junctional rhythm
Answer: d) Accelerated Junctional rhythm
Interpretation: The ECG rhythm includes a series of narrow QRS complexes, inverted P waves and a rate of about 70/minute. This rhythm originates from the AV junction. Because this rhythm occurs at rates faster than the junction typically fires (40-60/minute) but less than a tachycardia (100/minute), this ECG rhythm is called an accelerated Junctional rhythm.
10.
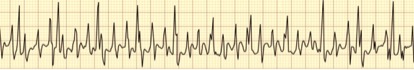
This ECG rhythm is:
a) Supraventricular tachycardia (SVT)
b) Movement artifact
c) Atrial fibrillation
d) Atrial flutter
Answer: b) Movement artifact
Interpretation: At a quick glance, this ECG rhythm appears to be a very rapid SVT with a rate near 300/minute. While this is possible (but unlikely), a more plausible explanation is that this is movement artifact caused by brushing one’s teeth, for example. Note the narrow QRS complexes with larger amplitude that occur regularly. These are probably an underlying SVT at a rate of about 110/minute.
11.
This ECG rhythm is:
a) Atrial fibrillation
b) Sinus rhythm with movement artifact
c) Atrial flutter with 2:1 ventricular response
d) Atrial flutter with variable block
Answer: d) Atrial flutter with variable ventricular response
Interpretation: The presence of the classic saw-tooth shaped flutter waves between the QRS complexes points to atrial flutter. In atrial flutter, the atria tend to beat at rates of about 300/minute. The ventricular rate is variable according to the variable block at the level of AV node.
12.
This ECG rhythm is:
a) Sinus tachycardia
b) Atrial fibrillation with rapid ventricular response
c) Junctional tachycardia
d) Ventricular tachycardia
Answer: c) Junctional tachycardia
Interpretation: This rapid ECG rhythm includes narrow QRS complexes, an absence of P waves prior to each QRS and a rate faster than 100/minute. This rhythm occurs at a rate of about 180- 190/minute. Notice the inverted waveform after many of the QRS complexes – possible further evidence for Junctional tachycardia (inverted P waves).
Note: At very rapid rates (>160/minute), the presence of P waves is often shrouded by the T waves. As a result, fast rhythms with narrow QRS complexes are comfortably called SVT (not an option with this question).
13.

This ECG rhythm is:
a) Sinus arrhythmia
b) Junctional rhythm
c) Junctional Bradycardia
d) Sinus Bradycardia
Answer: c) Junctional Bradycardia
Interpretation: This extremely slow rhythm includes narrow QRS complexes, no P waves and a rate of about 30/minute. This rhythm originates from the AV junction. Because this rhythm occurs at a rate slower than the junction typically fires (40-60/minute), this ECG rhythm is called a Junctional Bradycardia
14.

This ECG rhythm is:
a) Multifocal atrial tachycardia
b) Sinus tachycardia
c) Junctional tachycardia
d) Ventricular tachycardia
Answer: a) Multifocal atrial tachycardia
Interpretation: This rhythm might initially appear to be a ventricular tachycardia (VT) because of the wide QRS complexes or atrial fibrillation due to the rhythms irregular pattern.
This ECG rhythm is not VT due to its irregular pattern. Ventricular tachycardia generally follows a rapid regular pattern. The atrial fibrillation with aberrant ventricular conduction is also possible but at close inspection –the 1st, 2nd, 4th and 6th complexes for example – consistently shaped P waves are evident. At least three different P wave configurations are seen with this rhythm strip, leading to a claim that this is a multifocal atrial tachycardia.
15.
This ECG rhythm is:
a) Junctional tachycardia
b) Supraventricular tachycardia (SVT)
c) Sinus tachycardia
d) Atrial fibrillation with fast ventricular response
Answer: b) Supraventricular tachycardia (SVT)
Interpretation: This extremely rapid ECG rhythm includes narrow QRS complexes and a rate of about 270/minute. While this may only be movement artifact, assuming the patient is still and that the electrodes have good skin contact, this rhythm could be atrial fibrillation with rapid ventricular response, atrial flutter with a 1:1 ventricular response, atrial tachycardia and/or a consequence of Wolff-Parkinson-White syndrome for example. To be safe, the best answer is probably just supraventricular tachycardia (a classification that serves to include all of the previous mentioned rhythms).
16.
This ECG rhythm is:
a) Sinus arrhythmia
b) Wandering pacemaker
c) Sinus rhythm
d) Atrial fibrillation
Answer: b) Wandering pacemaker
Interpretation: A slower version of multifocal atrial tachycardia, the narrow QRS complexes, the various P wave configurations and an irregular rate of about 80/minute all support this ECG rhythm to be a wandering pacemaker. While this rhythm is slightly irregular (this is typical of sinus arrhythmia), the changing P waves is the most important finding. Note how the P waves are initially upright (sinus), then absent with inverted P waves buried in the QRS complex (Junctional), then biphasic (atrial) with unpredictable patterns thereafter (classic findings for a wandering pacemaker).
17.
This ECG rhythm is:
a) Sinus rhythm with aberrant intraventricular conduction and two PVCs
b) Atrial fibrillation with aberrant intraventricular conduction
c) Sinus rhythm with two PJCs with aberrant intraventricular conduction
d) Sinus arrhythmia with aberrant intraventricular conduction
Answer: c) Sinus rhythm with two PJCs
Interpretation: The underlying sinus rhythm presents with marginally wide QRS complexes, upright P waves and a rate of just less than 100/minute. The premature QRS complexes are narrow making these either premature atrial complexes (PACs) or premature Junctional complexes (PJCs). Looking carefully for clues, notice that the QRS complexes of these premature beats include a deeper inverted notch than the other QRS complexes. When taken together with the absence of any P waves before these premature QRS complexes, the evidence points strongly to premature Junctional complexes (PJCs).
18.
This ECG rhythm is:
a) Atrial fibrillation with rapid ventricular response
b) Accelerated Junctional rhythm
c) Sinus tachycardia
d) Junctional tachycardia
Answer: d) Junctional tachycardia
Interpretation: This rapid rhythm includes narrow QRS complexes, no P waves and a rate of about 150/minute. The absence of P waves suggests that this rhythm originates from the AV junction. Thus, this ECG rhythm is a Junctional tachycardia.
19.
This ECG rhythm is:
a) Wandering pacemaker
b) Sinus rhythm
c) Junctional rhythm
d) Accelerated idioventricular rhythm
Answer: c) Junctional rhythm
Interpretation: This rhythm could be a normal sinus rhythm except that the narrow QRS complexes are not accompanied by any P waves. Therefore, this rhythm that occurs at a rate of about 60/minute originates from the AV junction. Because this rhythm occurs at a rate characteristic of a Junctional pacemaker (40-60/minute), this ECG rhythm is a Junctional rhythm.
20.
This ECG rhythm is:
a) Atrial flutter with variable ventricular response
b) Sinus rhythm with PACs
c) Atrial fibrillation with fast ventricular response
d) Sinus arrhythmia
Answer: a) Atrial flutter with variable ventricular response
Interpretation: The saw-tooth flutter waves together with some regularity in its pattern give this ECG rhythm away. Note that the flutter waves occur at a rate close to 300/minute. The R-R intervals suggest rates of close to 100/minute (3:1 ventricular response), then 75/minute (4:1 ventricular response) and later a rate of 60/minute (5:1 response). The atrial flutter is presenting with variable AV blocking resulting in variable ventricular response.
21.
This ECG rhythm is:
a) Atrial flutter with multifocal PVCs
b) Atrial fibrillation with multifocal PVCs
c) Sinus Bradycardia with multifocal PVCs
d) Accelerated Junctional rhythm with PACs
Answer: b) Atrial fibrillation with multifocal premature ventricular complexes (PVCs)
Interpretation: This chaotic underlying ECG rhythm includes narrow QRS complexes and a rate of about 90/minute. The chaotic baseline displays coarse fibrillatory waves in keeping with atrial fibrillation (rather than the orderly saw-tooth pattern seen with atrial flutter). The wide premature QRS complexes present with at least two morphologies (shapes) making these multifocal PVCs.
22.
This ECG rhythm is called:
a) Sinus rhythm with a PVC
b) Sinus rhythm with a PAC
c) Accelerated Junctional rhythm with a PVC
d) Junctional tachycardia with a PVC
Answer: c) Accelerated Junctional rhythm with a PVC
Interpretation: The underlying ECG rhythm includes narrow QRS complexes, no P waves and a rate of about 80/minute. This rhythm originates from the AV junction. While not quite a tachycardia (>100/minute), this rhythm occurs at a rate quicker than the junction typically fires (40-60/minute) making this an accelerated Junctional rhythm. The wide and premature QRS complex without an accompanying P wave is a premature ventricular complex (PVC).
to view the answer to the question above
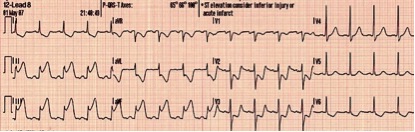
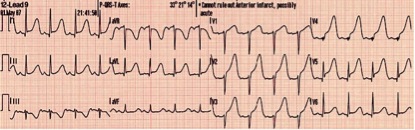
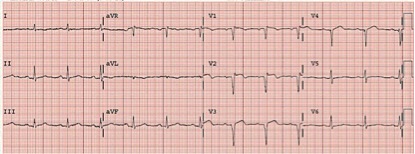
An inferior wall myocardial infarction (IWMI, inferior MI or inferior STEMI)
Occurs when inferior myocardial tissue supplied by the right coronary artery (RCA), is injured due to thrombosis of that vessel. When an inferior myocardial infarction extends to posterior regions as well, an associated posterior wall myocardial infarction may occur. The ECG findings of an acute inferior myocardial infarction include:
1.ST segment elevation in the inferior leads (II, III, and aVF).
2.Reciprocal ST segment depression in the lateral and/or high lateral leads (I, aVL, V5 and V6).
Note: If the reciprocal ST depressions are not present, consider alternative causes of ST segment elevation such as pericarditis.
The ST segment is the portion of the ECG from the end of the QRS complex to the beginning of the T wave. The ST segment normally remains isoelectric and thus ST segment depression or ST segment elevation can indicate cardiac pathology.
The ST segment is scrutinized on the ECG for the detection of myocardial ischemia. This can be done in the setting of exercise or pharmacologic stress testing as well.
Abnormal ST segments are reviewed based on the cause in the ECG criteria review sections and include anterior, posterior and inferior myocardial infarctions, left ventricular hypertrophy, pericarditis and Brugada syndrome.
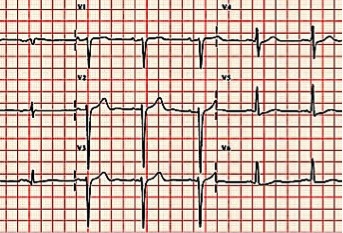
24.
to view the answer to the question above
An anterior wall myocardial infarction (AWMI or anterior STEMI)
Occurs when anterior myocardial tissue usually supplied by the left anterior descending coronary artery (LAD) suffers injury due to lack of blood supply. When an AWMI extends to the septal and lateral regions as well, the culprit lesion is usually more proximal in the LAD or even in the left main coronary artery. This large anterior myocardial infarction is termed an "extensive anterior".
The ECG findings of an acute anterior wall myocardial infarction include:
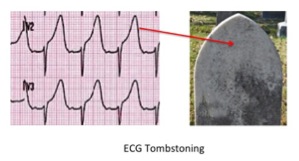
1. ST segment elevation in the anterior leads (V3 and V4) and sometimes in septal and lateral leads depending on the extent of the myocardial infarction. This ST elevation is concave downward and frequently overwhelms the T wave. This is called "tombstoning" due to the similarity to the shape of a tombstone.
2. Reciprocal ST segment depression in the inferior leads (II, III and aVF).
The ECG findings of an OLD anterior wall myocardial infarction include the loss of “anterior forces” leaving Q waves in leads V1 and V2. This is a cause of "poor R wave progression" or PRWP. Below is an example of an old anterior myocardial infarction:
Note: To distinctly say that an old anterior wall myocardial infarction is present on the ECG, there must be no identifiable R wave in lead V1 and usually V2 as well. If there is an R wave in V1 or V2, the term poor R wave progression can be used, but not an old anterior wall myocardial infarction.
On rare occasions, persistent ST elevation may be seen in V1 and/or V2 indicating a ventricular aneurysm, which is a known complication of a myocardial infarction. An example of an old anterior myocardial infarction with a left ventricular aneurysm is below:
Poor R wave progression refers to the absence of the normal increase in size of the R wave in the precordial leads as you progress from lead V1 to V6.
In lead V1, the R wave should be small. The R wave becomes larger throughout the precordial leads to the point where the R wave is larger than the S wave in lead V4. The S wave then becomes quite small in lead V6.
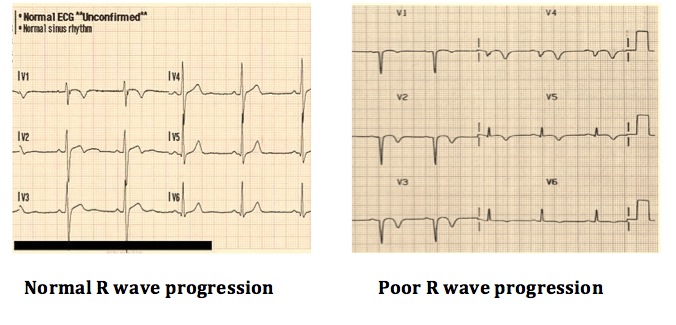
Note that an old anterior myocardial infarction can cause poor R wave progression. In this setting, there is no R wave in the anterior precordial leads and instead Q waves are present (see Anterior Myocardial Infarction).
The causes of poor R wave progression or PRWP are as follows:
1. Old anterior myocardial infarction 2. Lead misplacement (frequently in obese women) 3. Left bundle branch block or left anterior fascicular block 4. Left ventricular hypertrophy 5. WPW syndrome 6. Dextrocardia 7. Tension pneumothorax with mediastinal shift 8. Congenital heart disease
25.
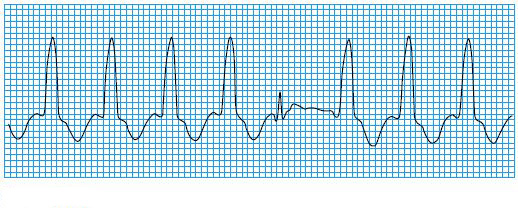
This ECG rhythm is called:
a) Sinus rhythm with a runs of PVC
b) VT with a capture beat
c) Accelerated Junctional rhythm with a PVC
d) Junctional tachycardia with a PVC
to view the answer to the question aboveb- VT with a capture beat
ECG waveform in VT is monomorphic. However, intermittently atrial breakthrough occurs before a ventricular beat has begun. This is referred to as a capture beat
26.

This ECG rhythm is called:
a) VT with a weak signal
b) VT with a fusion beat
c) Accelerated Junctional rhythm with a PAC
d) Junctional tachycardia with a PVC
to view the answer to the question above
b) VT with a fusion beat
- A fusion beat occurs when a supraventricular and a ventricular impulse coincide to produce a hybrid complex.
- It indicates that there are two foci of pacemaker cells firing simultaneously: a supraventricular pacemaker (e.g. the sinus node) and a competing ventricular pacemaker (source of ventricular ectopics).
- The fusion beats are of intermediate width and morphology to the supraventricular and ventricular complexes.
Causes
Fusion beats are seen with:
- Ventricular tachycardia
- Accelerated idioventricular rhythm (AIVR)