MCQ Self assessment
The following questions (#1-5) relate to the scenario below
A 62-year-old man has been admitted to a medical ward following a chest infection 2 days ago. He has a history of hypertension and diabetes. He complains of shortness of breath and “just not feeling right”. He then suddenly becomes unresponsive in front of you. Upon examination, you find he has no pulse. An Automated External Defibrillator (AED) is available on the ward.
1. Which of the following actions should be considered first?
a) Call for help then start chest compressions
b) Commence rescue breathing
c) Call for or send for help and the AED
d) Call for help and insert an IV
2. When you attach the bag-valve-mask device with a reservoir to the oxygen source, what is the correct flow rate to administer oxygen?
a) 4l/min
b) 6l/min
c) 8l/min
d) 10l/min
3. When the AED is available at the bedside, you need to:
a) Continue CPR for 2 minutes before analysing
b) Attach pads in preparation for the arrival of the resuscitation team
c) Turn on, follow prompts
d) Be prepared to shock after administration of first dose of Adrenaline
When the manual defibrillator is available the following rhythm is noted:

4. The patient has received the initial two shocks at 200J.
What medication would you consider at this time?
a) Atropine 0.5 mg IV
b) Adrenaline 1mg IV
c) Amiodarone300mgIV
d) Adenosine 6 mg IV
5. What is the correct ratio of compressions to ventilations for this non-intubated
patient?
a) 5 compressions to 1 breath
b) 30 compressions to 2 breaths
c) 3 compressions to 1 breath
d) 15 compressions to 2 breaths
The following questions (#6-9) relate to the scenario below
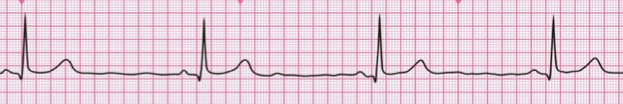
A 43 year old woman has been admitted to the emergency department stating she has palpitations, and feels a bit light headed. Her BP is 110/50. The monitor shows:

6. Which of the following is indicated first?
a) Adenosine 6mg IV
b) Perform Vagal manoeuvres
c) Give Verapamil 2.5mg IV
d) Sedation and immediate synchronised cardioversion
7. Your initial intervention has been ineffective in terminating this arrhythmia. An IV
has been established. What drug should be administered IV?
a) Adenosine 6mg
b) Amiodarone 150 mg over 10 min
c) Adrenaline infusion 2-10 micrograms/min
d) Adenosine 12 mg
8. The drug administered above has also been ineffective in terminating this
arrhythmia. What is the next drug that should be administered IV?
a) Adenosine 6mg
b) Amiodarone 150 mg over 10 min
c) Adrenaline infusion 2-10 micrograms/min
d) Adenosine 12 mg
9. The patient now states she is more short of breath and thinks she is going to faint.
Her BP is 86/50. Your next intervention will be:
a) Adenosine 6mg IV
b) Amiodarone 150 mg over 10 min
c) Give Verapamil 2.5mg IV
d) Sedation and immediate synchronised cardioversion
The following questions (#10-11)relate to the scenario below
A 73 year old man had been admitted to the medical ward with a chest infection. He has
rung his bell. When you came in, he was poorly responsive. He does have a weak brachial pulse. His BP is 88/60. He has oxygen and an IV line in place. The defibrillator has been attached, using the pads. The rhythm shown is:
10. The next treatment you will initiate is:
a) Dopamine infusion 10-20 microgram/kg/min and titrate to effect
b) Adrenaline 2-10micrograms/min and titrate to effect
c) Atropine 0.6mg IV up to a total dose of 3mg and prepare for TCP
d) Isoprenaline 2-10micrograms/min infusion titrated to effect
11. In preparing for TCP, you will need to:
a) Synchronise the manual defibrillator
b) Place the defibrillator in AED mode
c) Attach the 3-lead cable to obtain a tracing
d) Attach bedside monitor in addition to the manual defibrillator
The next questions (#12-18) relate to the following scenario
A 55-year old man presents to a GP clinic complaining of chest tightness and shortness of breath. He appears pale and states he feels “dizzy”. His blood pressure is 110/70mmHg.
His ECG is below.
12. Which of the following statements best describes the following ECG?
a) There are no acute ECG changes
b) There are acute changes consistent with a Non-ST Elevation Myocardial
Infarction
c) There are acute changes consistent with a ST-Elevation Myocardial Infarction
d) There are ECG changes consistent with LBBB
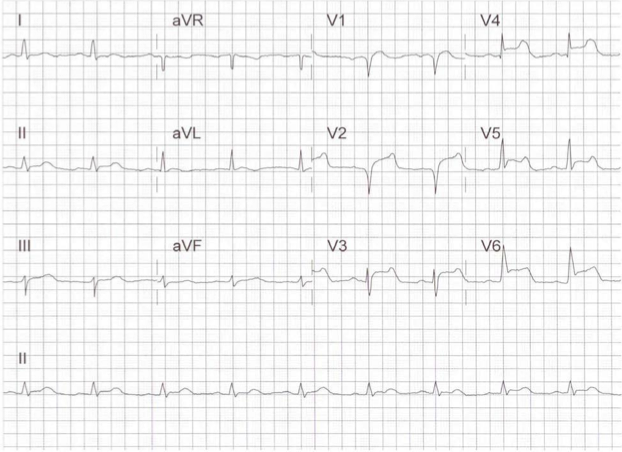
13. Which of the following treatments are not required for the immediate management
of this patient’s Acute Coronary Syndrome?
a) High flow oxygen therapy
b) Aspirin PO
c) Nitro-glycerine spray 0.4mg SL
d) Glycoprotein IIb/IIIa Inhibitors
14. What is the correct dose of Aspirin to be administered?
a) 10-50mg
b) 50-100mg
c) 150-300mg
d) 600mg-1.2mg
15. After initiating the immediate management, the patient’s chest pain has been
resolved. His BP has remained 110/70. Which of the following interventions is most
important in reducing in-hospital stay and 30 day mortality rate?
a) Reperfusion therapy
b) Transcutaneous pacing (TCP)
c) Repeat aspirin 325mg orally
d) A beta blocker
16. After several minutes the patient complains of worsening pain and then suddenly
can no longer be roused. A pulse check reveals that he has no pulse. The monitor
shows the following rhythm:

Which of the following treatments should be considered first?
a) Endotracheal intubation
b) Defibrillation
c) Cardioversion
d) Transcutaneous pacing
17. After the second shock, the monitor shows:

High quality CPR is in progress.
What medication would you give next?
a) Adrenaline 1mg IV
b) Amiodarone 150mg IV
c) Adenosine 6mg IV
d) Amiodarone 300mg IV
18. What is the correct rate of compressions per minute for this patient?
a) 80 per minute
b) 90 per minute
c) >120 per minute
d) 100 - 120 per minute
19. What is the correct dose of adrenaline to be administered intravenously?
a) 3mg every 3 minutes
b) 2mg every 3minutes
c) 1mg every 3 minutes
d) 0.5mg every 3 minutes
20. What are the ABCD assessments of the BLS Primary Survey?
a) airway, blood pressure, circulation, defibrillation
b) airway, breathing, compressions, defibrillation
c) air, breathing, cardiac arrest, defibrillation
d) airway, breathing, circulation, differential diagnosis
21. What are the ABCD assessments of the ACLS Secondary Survey?
a) airway, blood pressure, circulation, defibrillation
b) airway, breathing, circulation, defibrillation
c) air, breathing, cardiac arrest, defibrillation
d) airway, breathing, compressions, differential diagnosis
22. How often should an adult patient be ventilated if they are experiencing respiratory arrest?
a) >30 times per minute
b) 8 to 10 times per minute
c) 10 to 12 times per minute
d) 18 to 22 times per minute
23. What are the risks associated with Hyperventilation?
a) Decreased venous return to the heart
b) Diminished cardiac output
c) Increases intrathoracic pressure
d) All of the above
24. The target oxygen saturation that should be maintained in ACS is
a) 88%
b) 94%
c) 99%
d) any concentration above 80%
25. Which basic airway skill is the most commonly used method for providing positive-pressure ventilation?
a) Mouth-to-mouth
b) Mouth-to-barrier device
c) Bag-mask ventilation
d) A time cycled ventilator
26. A Rigid Catheter type is more effective than a Soft Catheter type for which of the following uses:
a) More effective suctioning of the oropharynx
b) Aspiration of thin secretions from the oropharynx and nasopharynx
c) Performing intratracheal suctioning
d) Suctioning through an in-place airway to access the back of the pharynx in a patient with clenched teeth
27. One cycle of CPR consists of
a) 30 compressions then 2 breaths
b) 20 compressions then 2 breaths
c) 30 compressions then 3 breaths
d) 20 compressions then 3 breaths
28. When using a monophasic defibrillator, how many joules should be delivered for one shock?
a) 270-J
b) 320-J
c) 360-J
d) 390-J
29. Which one of the following is not a common cause of PEA?
a) Hypoxia
b) Hyperglycaemia
c) Toxins
d) Thrombosis
30. Which of the following are the two most easily reversible causes of PEA?
a) Hypovolemia and PE
b) Thrombosis and chest Trauma
c) Hypoglycemia and Hypoxia
d) Tension pneumothorax and Hyperkalaemia
31. Cardiac arrest rhythm associated with no discernible electrical activity on the ECG is
a) VF
b) Bradycardia
c) Pulseless Electric Activity
d) Asystole
32. Which of the following is not a recommended agent to be administered to patients under evaluation for ACS?
a) Morphine
b) Epinephrine
c) Aspirin
d) Nitroglycerin
33. Which of the following is a standard treatment procedure for patients with STEMI?
a) Reperfusion therapy
b) Use of a soft catheter
c) Defibrillation
d) Administration of morphine
34. TCP is not a recommended treatment for which of the following?
a) Standby pacing
b) Bracycardia with escape rhythms
c) Asystole
d) Hemodynamically significant bradyarrhythmia
35. Which of the following agents may be be administered to patients under evaluation for unstable tachycardia?
a) No agents are recommended
b) Midazolam
c) Oxygen
d) Aspirin
36. Which of the following is not a symptom of unstable tachycardia?
a) Shortness of breath
b) Hypertension
c) Altered mental status
d) Chest pain
37. Fill in spaces a-g:
Select from the following: Adrenaline IM. 0.5mg, Saline, adrenaline 1mg IV/IO, isoprenaline, aminophylline, antihistamine, 10 mcg/kg, 5 minutes, 10 minutes, 1000 , 2000, 20,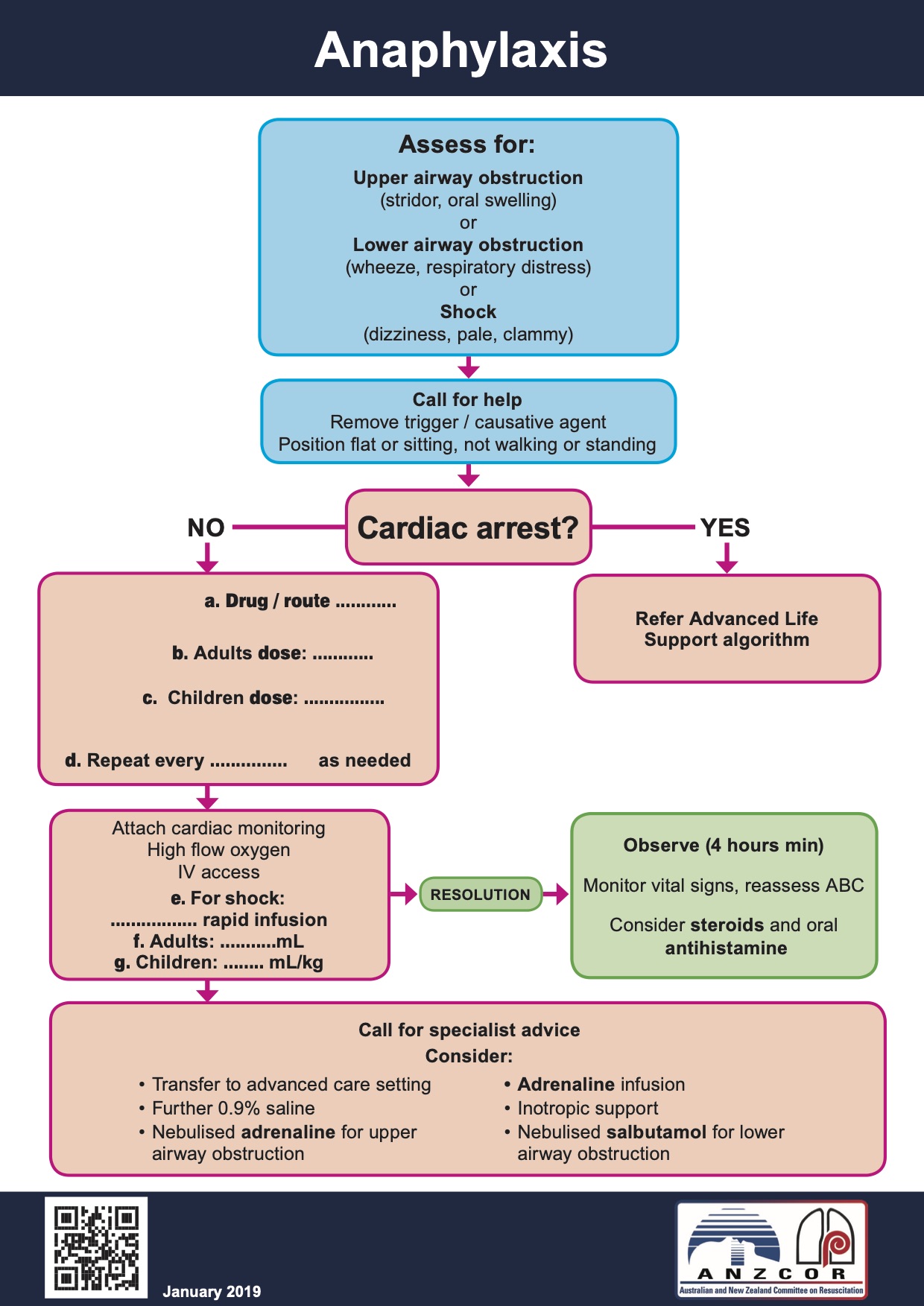
to view the answer to the question above
a: adrenaline IM
b: 0.5 mg
c: 10 mcg/kg
d: 5 minutes
e:Saline
f: 1000
g: 20
38. A 28 years old male presented with palpitations and severe dizziness. Symptoms started 4 days ago. He is a known case of WPW (Wolf Parkinson White). His blood pressure is 70/42 mmHg. His ECG shows a wide complex tachycardia with irregular irregulatory pattern.
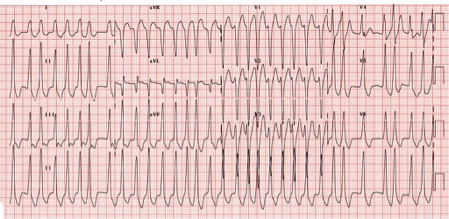
What is the best treatment?
a) DC cardioversion
b) Adenosine IV
c) Verapamil IV
d) Amiodarone IV
Correct answer is a. This is an Atrial Fibrillation transmitted directly through the abberent pathway to the ventricles (hence a wide complex). Treatment is for an unstable tacycardia which is immediate cardioversion. Risk of embolisation is possible as this condition started 4 days ago.
40. Which of the following diagrams shows the correct placement of the pacing pads:
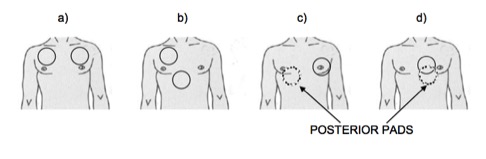
Correct answer is "d"
41. Which of the following statements are possible positions of the defibrillation pads on this patient?
- One pad to the right of upper sternum below the right clavicle and the other in mid axillary line at level of V6
- One pad anterior to left precordium and the other inferior to left scapula (antero-posterior)
- One pad in mid axillary line at level of V6 and the other over the right scapula (Postero-lateral)
- Bi-axillary on either side at mid axillary line
a) 1 & 2
b) All are acceptable positions
c) 1, 2 & 3
d) 1 & 4
Fill in the blanks:
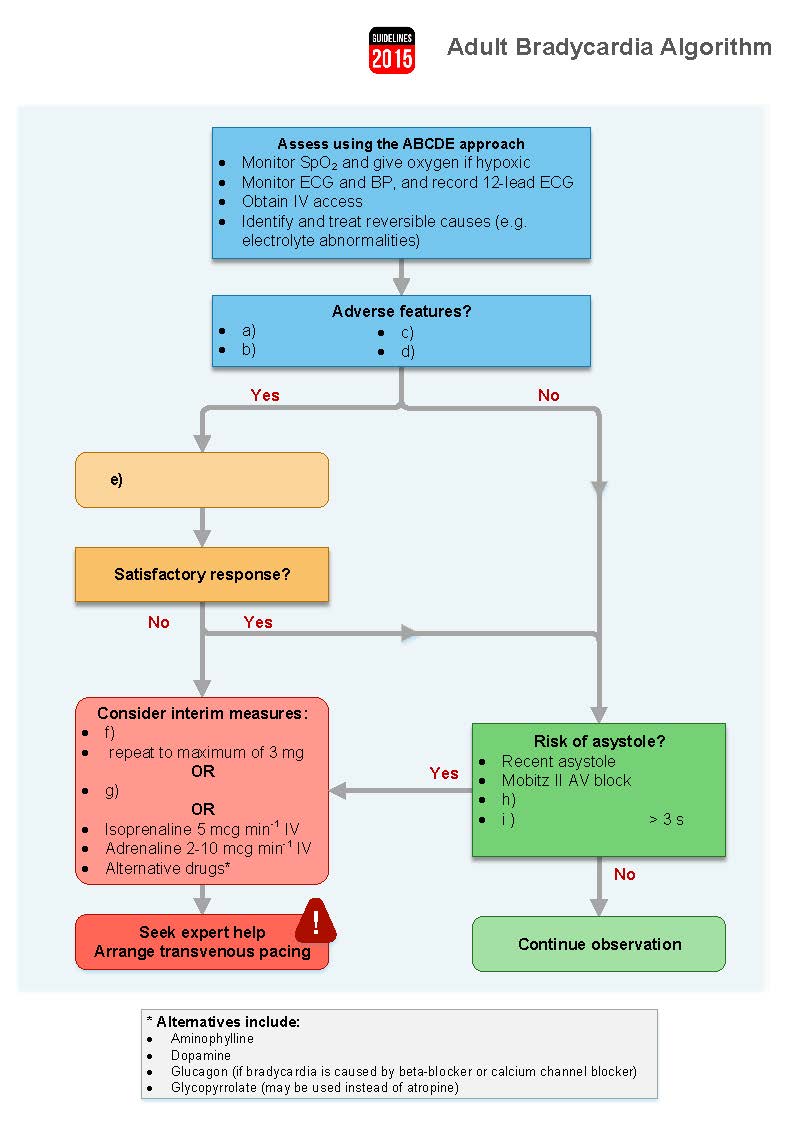
a: shock
b: syncope
c: myocardial ischaemia
d: heart failure
e: Atropine 500/600 mcg IV
f: Atropine 500/600 mcg IV
g: TCP
h: Complete heart block with broad complexes
i: Ventricular pause




